Indian Journal of Health Social Work
(UGC Care List Journal)
ASHA WORKERS IN INDIA: THEIR CONTRIBUTIONS, CONSTRAINTS,
AND PATHWAYS FOR IMPROVEMENT
Avantika Singh1 & Looke Kumari2
1Assistant Professor, Department of Political Science, University of Delhi, 2Assistant Professor,
Department of Political Science, Bharati College, University of Delhi
Correspondence: Avantika Singh, e-mail: asingh@polscience.du.ac.in
ABSTRACT
Community Health Workers as a crucial social engineering for attaining the goal of Universal
Health Coverage has become the norm in underdeveloped and developing countries since the
early 2000s. As the goals of attaining healthcare objectives intersected with the larger goal of
achieving gender equality, the centrality of women in spearheading such initiatives was
acknowledged with great enthusiasm. This article attempts to formulate a diversified
understanding of the functions of Community Health Workers (CHW) within the context of the
Accredited Social Health Activist (ASHA) in India. The larger objective is to understand the unique
role of ASHA workers in contributing to India’s healthcare objectives, easing the accessibility of
marginalized masses, and assessing the associated challenges. It also highlights the agency of
ASHA in the state and the way forward to make the system more robust.
Keywords: Primary Health care, Community Health Workers, ASHAs, COVID-19
INTRODUCTION
Since the welfarist development model
started gaining traction among the democratic
and socialist regimes worldwide, the idea of
delivering essential services to marginalized
social groups became prominent. The welfare
regime implies a mandate to provide social
assistance for the populace’s fundamental
sectors like health, education, employment,
and pension. The social security mandate is
one of the hallmarks of the welfare state. The
Constitution of India reflects these provisions.
India, a nation that accounts for 17% of the
global population, is responsible for 19% of
global maternal fatalities and 21% of global
juvenile deaths. Nevertheless, it has made
substantial contributions, particularly since the
introduction of the National Rural Health
Mission (NRHM) program in 2005. “NRHM
contains a variety of strategies and schemes,
such as a conditional cash transfer scheme,
an emergency transport mechanism,
i mproved communitization through the
establishment of Village Health, Sanitation,
and Nutrition Committees (VHSNC), and
investments in health infrastructure and
health workforce, which include the
establishment of a new cadre of community
health volunteers as ASHAs” (Sheila C. Vir,
2023).
National Rural Health Mission (NRHM)
It was introduced in April 2005 as an India
for Health project to enhance service quality
at the primary and secondary levels. The Ministry of Health administers this program.
The Mission aims to establish a completely
community-owned centralized healthcare
delivery system. The objective is to deliver
accessible, cheap, and accountable quality
healthcare services in rural regions. NRHM is
acknowledged as the principal initiative
encompassing all current Health and Family
Welfare programs, including “Reproductive
Child Health-2 (RCH-2), the National Malaria
Control Programme, Tuberculosis (TB), Kala
azar, Filaria, Blindness, Iodine Deficiency, and
Integrated Disease Surveillance. The Mission
is a program sponsored by Central Resources”
(Enisha Sarin et al., 2017).
The structure of the annual budget determines
the share of funding that the project would
receive. The NRHM program necessitates the
states to increase by 10% their public health
budget each year. The primary healthcare
services were extended to urban areas in
2013 when the National Urban Health Mission
(NUHM) was introduced. ASHA workers’ role
is vital in the success of such initiatives.
Hence, ASHA, the flagship extension of the
NRHM, serves as a foundational pillar for
overcoming the enduring challenges of
accessing healthcare for the rural population.
Definition of Community Health Workers
(CHWs)
They are individuals from the local community
who get monetary incentives for volunteering
to deliver health services to rural and urban
areas in tandem with the existing local system
in health care. CHWs are the first line of
defense as health professionals in the
healthcare system, with an extensive
understanding of the population they serve.
A crucial connection to healthcare systems at
the grassroots level is that they serve as an
essential bridge between the healthcare
system and their communities (Ballester,
2005). This can enhance access to healthcare
services in isolated regions.
CHWs have global recognition, originating
from community-based healthcare initiatives.
The World Health Organization, in its Alma
Ata Declaration of 1975, formally recognized
CHWs as a general designation, defining their
global role and emphasizing the critical role
of healthcare services at the primary level.
‘Health for All’ was a mission directive by the
World Health Organisation (WHO). It aims to
catalyze community development, raise
knowledge about health services and their
significance, and directly deliver healthcare.
In order to provide women in their
communities with essential and nutritional
services, CHWs are often members of the
local community who have undergone minimal
training (Walt, 1989). They usually work
intermittently as healthcare providers and are
expected to stay in their native areas.
CHWs are crucial in bridging the healthcare
system and community gap. Their
interventions are often more effective than
t hose driven solely by healthcare
professionals in identifying and leveraging the
community’s strengths to promote health
improvement (Bishop C et al., 2002). CHWs
can understand, harness, and maximize the
community’s resources, leading to enhanced
health outcomes through improved access and
cultural engagement, particularly for
underserved populations.
Despite the Indian Government’s commitment
to enhancing healthcare in rural regions
through NRHM, delivering adequate health
services remains a significant challenge. It is
crucial to recognize the need for improved
training and resources for ASHA workers at
the forefront of this Mission.
In 2002, Chhattisgarh introduced an
innovative community health care model by
appointing women as Mitanin, or Community
Health Workers. These women served as
intermediaries for marginalized groups,
bridging the gap between the needs of local
populations and distant health systems. The national government launched the Accredited
Social Health Activist (ASHA) program in
2005-06 as part of NRHM, which was later
expanded to urban areas by establishing the
National Urban Health Mission in 2013.
Accredited Social Health Activist (ASHA)
NRHM in India established the ASHA program
in 2005 to enhance women’s engagement in
specialized work attendance. ASHAs are
chosen from the local community and are
committed to providing healthcare facilities.
They are instructed to link the public health
care system and the local community. The
subjects are predominantly rural women
between the ages of 25 and 45 who have
completed up to Class 10. Typically, there is
one ASHA per 1,000 individuals. This ratio may
be adjusted to one ASHA per residence in
tribal, hilly, and arid regions, contingent upon
the workload.
Joshi, R.S., and George, M. (2012), from
Thane district, Maharashtra, highlight the
diverse role of ASHA workers within the health
system as “agents of change,” encompassing
awareness, health services, family planning,
and the door-to-door dissemination of
information regarding maternity schemes and
child development programs. According to the
Policy Brief (2018), India is ranked 150th out
of 153 nations regarding women’s health and
survival, indicating poor standing. The survey
also reveals that domestic violence against
women in Western India exceeds that
experienced by 82% of males. In this context,
ASHA workers offer counseling, attentively
consider women’s circumstances, provide
guidance, and enhance their awareness,
especially when family members exhibit
conservative tendencies. Additionally, ASHA’s
primary tasks include “advocating for prenatal
and postnatal services, facilitating institutional
births, promoting regular vaccination in
children, distributing condoms and oral
contraceptive pills, and encouraging healthy
behaviors within communities” (USAID India,
2008).
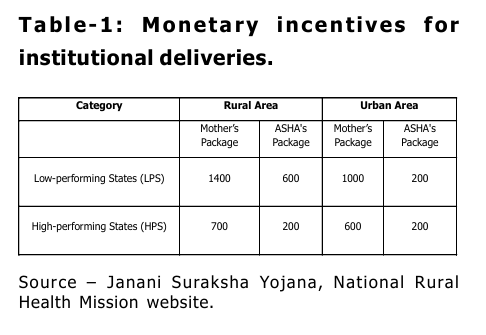
The national Janani Suraksha Yojana (JSY)
impacts ASHAs and new mothers significantly.
Under this mandate, most ASHAs advocate for
institutional delivery, incentivizing institutions
to deliver services. A new mother in a rural
area is entitled to Rs. 1400 and Rs. 700 in
different state settings. ASHAs receive Rs. 600
and Rs. 200 as an incentive for institutional
birth. In urban settings, a new mother is
entitled to Rs. 1000 and Rs. 600, while ASHAs
receive Rs. 200 as an incentive for institutional
birth (Table 1)
ASHA is a critical organization in the
Anganwadi community, as it promotes health
awareness, provides medical care, and
encourages community involvement. They
guide various health-related matters,
including diet, lifestyle, and work-related
circumstances. In addition, they establish a
local health plan and enable children and
expectant mothers to access medical care at
their convenience. Anganwadi officials conduct
meetings with ASHA workers, function as
reference persons for training, and provide
them with information about outreach
sessions. Additionally, they guarantee that
employees receive compensation and
participate in training. ASHA also organizes
health days at the Anganwadi Center.
The ASHA program requires ASHAs to act as
“link workers,” facilitating the connection between rural residents and health service
facilities. They serve as “service extension
workers,” providing instruction and essential
materials to encourage the preservation of
life.
ASHA workers occupy a very unique role in
making healthcare accessible to the most
marginalized and vulnerable communities.
They significantly contribute to raising
awareness on health-related issues,
mobilizing local communities for healthcare
planning, and ensuring accountability and
proper utilization of existing healthcare
infrastructure.
Their role is essential in reducing the maternal
mortality rates (MMR) in India. According to
the Sample Registration System’s (SRS) data
(2022), the mortality rate was 374 deaths per
100,000 live births from 2014 to 2016, which
declined to 97 fatalities per 100,000 live births
from 2018 to 2020.
ASHA has contributed to this significant
reduction in several ways: (a) By facilitating
hospital deliveries and providing prenatal and
postnatal care, (b) by regularly paying home
visits to pregnant women for their health
assessment and detect any possible
complications, (c) disseminating knowledge
related to women’s health and guide during
crises, (d) collaborating with governmental
programs to improve healthcare accessibility
such as Janani Suraksha Yojana (JSY) which
provides monetary incentives for mothers and
promotes hospital births, (e) enhancing
community spirit, addressing socio-cultural
barriers and raising awareness on health
related matters. Consequently, hospital births
in India saw a significant rise from 78.9%
(National Family Health Survey (NFHS)-4, 2015
to 16) to 88.6% (National Family Health
Survey (NFHS)-5, 2019 to 21). Moreover, the
MMR significantly decreased from 556 per
100,000 live births in 1990 to 103 per 100,000
live births in 2022.
In the same spirit, ASHA workers have also
contributed to decreasing malnutrition among
children aged five and below. The NFHS-4
(2015 – 2016) reported the malnutrition level
to be 38.4%, which was reduced to 35.5% in
NFHS-5 (2019-2021). They effectively
contribute in promoting neonatal care
practices and guiding families on the
importance of breastfeeding. This contributed
to the drastic decrease in the Infant Mortality
Rate (IMR) in India from 89 per 1000 live
births in 1990 to 27 per 1000 live births in
2022. Furthermore, ASHA workers
disseminate knowledge on the importance of
getting vaccinated and address reluctance
regarding vaccines among the populace. They
were involved in conducting door-to-door
visits, organizing village meetings, and
engaging in health campaigns to notify people
about the schedule for vaccination, especially
for children under two. They actively engaged
in the government’s flagship program, Mission
Indradhanush (2019). The objective of the
Mission was to achieve comprehensive
vaccination coverage for all children under two
years and pregnant women. ASHA workers
were equipped with digital instruments like
the MCTS to track mothers and children and
the RCH portal, where information about
vaccination coverage and schedules could be
monitored. The significant contribution of
ASHAs leads to a dramatic increment in India’s
comprehensive vaccination coverage for
children 12 to 23 months old, from 62% in
NFHS-4 (2015 to 16) to 76.4% in NFHS-5
(2019 to 21). This remarkable achievement
is accredited to the direct engagement of the
ASHA workers in ensuring that children
adhered to the prescribed vaccination
schedule, including those for diphtheria,
pertussis, tetanus (DPT), polio, measles, and
other preventable diseases. Enhanced
vaccination coverage can be directly
correlated with the reduction in child mortality
rates as reflected in the assessment of IMR, which is decreased compared to the national
average in regions where ASHA workers were
highly active, namely Kerala, Tamil Nadu, and
Himachal Pradesh.
In 2022, Kerala’s IMR was substantially lower
than the national average of 27 per 1,000 live
births, at just 6 per 1,000. In the
underprivileged districts targeted by the
Aspirational Districts Programme, where IMR
was previously high, ASHAs have played a
crucial role in enhancing healthcare delivery,
resulting in noteworthy declines in infant
mortality.
However, there has been substantial research
that has critically mapped the performance
of ASHA. Jan exhibited sub-par performance
in the immunization program, wherein the
health workers required a better
understanding of the dosages of common
medications. In a seminal work, Mahyavanshi
et al. (2011) investigated the knowledge,
attitudes, and practices of ASHA workers
related to child health in Surendranagar
district, Uttar Pradesh, revealing that 86.2%
of ASHAs possessed inadequate knowledge
about newborn care, while 90% were
unaware of the appropriate advice to provide
mothers for preventing hypothermia and
administering Kangaroo Mother Care. Seventy
percent of individuals were aware of the signs
of diarrhea, although 91.5% were uninformed
about the indications of dehydration; also,
68.46% lacked knowledge regarding measles
and pneumonia. 96.92% of ASHA staff had a
positive attitude. Furthermore, he mentioned
that although ASHAs receive training, there
i s still room for improvement in their
understanding of various aspects of childhood
illness and mortality. Therefore, enhancing
the frequency and quality of training for ASHAs
is essential.
COVID and ASHA
ASHA workers were crucial to India’s COVID
19 response, particularly in rural regions, by
doing health surveillance, contact tracing, and
public health education. Over 1 million ASHA
workers engaged in pandemic-related
activities, including door-to-door surveys and
identifying possible COVID-19 cases. They
significantly contributed to implementing
vaccination programs, which increased
vaccination rates in rural areas of India.
However, they also encountered significant
vaccine reluctance (Nair, 2024). Nevertheless,
numerous ASHAs needed to be more
adequately equipped with the appropriate
personal protective equipment (PPE).
Research indicates that 60% of them lacked
sufficient personal protective equipment (PPE)
during the early phases of the COVID outbreak
(Mishra & Rai, 2021). The workload for ASHA
employees experienced a significant increase,
and some of them worked extended hours for
minimal pay based on their success, with an
average of only INR 2,000 to 4,000 per month
(Ghosh, 2021). Despite their challenges, their
efforts to improve sanitation, implement
quarantines, and provide information
significantly reduced the virus spread in rural
spaces, highlighting their importance during
the pandemic (ibid).
The usage of ‘war’ analogies in public
discourse during the COVID-19 epidemic had
a significant impact on the perceived duties
of community health workers in India,
particularly ASHA workers. Political leaders
used war metaphors to explain the
complexities of the epidemic and encouraged
public participation by portraying COVID-19 as
an adversary that required a collective
response (Bates, 2020). These metaphors
utilized familiar concepts such as enemy,
combatant, and home spaces to support
specific policy actions and evoke a sense of
urgency, concern, and danger (Flusberg et al.,
2018). This portrayal presents healthcare
workers as “soldiers” in the fight against the
disease. As a result, they are expected to
follow the directives of their superiors and recognize that specific individuals may be
injured or required to sacrifice for the greater
good of the group (Taylor & Lohmeyer, 2020).
The political aspects of the employment of
ASHA employees were brought to light by the
COVID-19 outbreak. The government failed to
adequately address their requests, even
though they were extolled as “frontline
warriors” for administering public health at
the local level. A significant number of ASHAs
were compelled to work without adequate
personal protective equipment (PPE) and risk
pay due to the ongoing risk of long-term viral
transmission (Nanda, 2020).
However, the research indicates that the
COVID-19 epidemic has altered the role of
hope, possibly generating new chances for
individuals to reconfigure their agency and
interactions with the state. Conventional
narratives emphasize female responsibilities,
but new discourses around pandemic-related
securitization may affect the subjectivity of
community health workers in unprecedented
ways (Pfrimer & Barbosa, 2020). The public
image of impermanent workers, equal pay for
men and women, and worker rights are all
interconnected with the politics of ASHA
workers. These concerns necessitate an
examination of the future of healthcare work
within India’s political and social framework.
LIMITATION
The ASHA program has been extensively
researched since its inception; however, its
implementation could be more consistent at
the state level due to stakeholders’ varying
perspectives and notions. ASHAs must
possess comprehensive knowledge and
i mparted training for their numerous
responsibilities in various Indian contexts to
fulfill their obligations effectively. In a nation
as varied as India, it is essential to
comprehend the primary health facilities
linked to ASHAs. They need to be better
furnished with sufficient facilities. Moreover,
little and unregulated financial incentives are
provided to aspirants, which tend to dissuade
rather than encourage them (Saprii L. et al.,
2015).
CHWs have proven to be effective worldwide
in several areas related to mother and child
health, including the encouragement
to breastfeed by new mothers, timely and
proper vaccination, critical care for newborns,
health education, and reduction in IMR and
MMR (Enisha Sarin et al., 2017). Nevertheless,
challenges persist in the performance of
CHWs. Glenton C. et al. (2013) identified
organizational, social, and interpersonal
factors facilitating or impeding community
health. Although social acceptability and
organizational support were essential for
CHWs, the program’s effectiveness obstacles
were linked to the interactions between
beneficiaries and the health system, existing
socio-cultural factors, and institutional
variables (Enisha Sarin et al., 2017). The
socio-cultural norms regulating the services
of female CHWs have been deemed as
essential for the proper execution of their
duties (Khan, MH et al. 2006).
Interpersonal
barriers
encompass
interference leading to fear of blame in the
event of failure due to delays in accessing
healthcare facilities, time constraints, inability
to fulfill community needs, or a lack of
understanding. All of these may effectively
hinder the work of ASHA, who are locally
situated women and know the community well.
Additionally, ASHA workers might be a target
of community members due to Institutional
hurdles, which may encompass restricted
supplies (Low, L.K., et al. 2006), unnecessary
documentation (Javan Parsant, 2009), and
inadequate assistance from a rigid and
hierarchical healthcare system (Scott, K,
2010).
The role of ASHAs within India’s health system
and labor initiatives is deeply intertwined with
the political landscape in which they operate. Their role as informal leaders in the
healthcare domain situates them at the
crossroads of labor rights, gender politics, and
public health. The ASHA workers have
contributed significantly to the national
agenda of public health initiatives like the
National Health Mission (NHM). However, it has
been noted that the official label of
“volunteers” for the ASHA workers puts them
in a vulnerable position regarding monetary
compensation, labor rights, and societal
recognition (Scott, 2019). The official
designation of “volunteers” implies that the
monetary compensation of the ASHA workers
would be based on performance-based
incentives. The denial of a fixed salary
package and the uncertainty of receiving
regular income contributed to the widespread
dissatisfaction among the ASHA workers. It
was highlighted that their income often falls
below the subsistence level threshold,
typically between INR 2000 and 4000 per
month (Nandi & Schneider, 2020). Despite
their substantial contributions to the public
health objective and their tireless work for
public services, denying a formal work
designation excludes ASHA workers from the
protection and benefits of many social security
nets like labor laws, health insurance,
pensions, and so on.
The gendered demography of the ASHA
workforce, which is an all-women collective,
essentially implicates them within the broader
issues of gender inequality, such as the
undervaluation of care work and societal
expectations for women to undertake
caregiving roles. These narratives of
unrecognized labor necessitate them to
organize politically and meet the demands of
formalizing their work or providing adequate
financial compensation (Ved, 2019). Their
selfless contributions throughout the horrors
of the COVID pandemic justify their demands
for the formalization of work, enhanced
monetary compensation, legal contracts, and
greater inclusion in the social security
systems (Ghosh, 2021).
CHWs in underdeveloped and developing
countries are subjected to significant stress
stemming from job demands, inadequate
remuneration, poverty, gender discrimination,
and their position at the lower echelons of
systemic hierarchies. These risks are further
intensified by circumstances such as a family
member’s unemployment, children’s
education, a history of mental illness, and
marital discord. ASHAs must regulate their
emotions in response to job pressures and
interact with diverse community members and
the health system. They engage with
beneficiaries and their families in the
combined capacity of an advisor and health
care provider, potentially exhibiting a
spectrum of emotions, from elation to grief.
Knowledge, Attitude, Encouragement,
and Additional Skills of ASHA Workers:
Way Forward
Dieleman M. et al. (2003) state, ‘ to ensure
high-quality healthcare services, it is essential
t o formulate strategies that enhance
employee motivation for improved
performance.’ Research suggests that while
financial incentives are significant, they are
i nsufficient to enhance employee
performance. Various performance
management techniques may accomplish this.
Further, Dieleman M. et al. (2003) observed
in their study that acknowledgment is crucial
for healthcare worker supervisors, colleagues,
and the community. Mundhra (2010)
categorizes motivation as extrinsic and
i ntrinsic motivation. External elements
quantifiable in monetary terms, like salary and
bonuses, are defined as extrinsic motivation.
Intrinsic Motivation manifests via qualities
such as interest, enjoyment, preference, and
perceived aptitude. Wichita et al. (2007)
highlight Motivation, attitude, and aptitude as
crucial for good outcomes. The socio-cultural norms regulating the services of female
Community Health Workers have been
recognized as essential for the proper
execution of their duties (Khan, M.H et al.
2006).
Franco and colleagues (2002) established a
conceptual framework for elucidating worker
motivation, which this article reflects upon.
This framework identifies internal and
external elements like self-concept, social
i nfluences, organizational systems, and
structures. Culture and community may serve
as motivating variables in assessing employee
motivation. One cannot operate in opposition
to the culture that influences one’s capacity
to execute organizational support frameworks
and fundamental procedures (Franco. LM et
al., 2002).
Further, the article bases its argument on the
NCHA’s (National Health and Advisory, 1998)
work, whose research indicated that CHWs
should possess proficient communication
abilities, instructional and presentation skills,
advocacy, organizational service coordination,
and a comprehensive understanding of the
social service system. CHW needs continuous
training and supervisory assistance to make
practical judgments during crises.
Occasionally, healthcare professionals possess
the capability to fulfill their duties but may
need more drive to exert the necessary effort
to complete all essential tasks. Worker
motivation denotes an unactualized process
that influences behavior’s direction, intensity,
and persistence (Vroom, 1996). Individual
Motivation and sufficient support from
executives and coworkers influence employee
performance (Mishra, 2014).
REFERENCES
Ballester, G. Community Health Workers:
Essential to Improving Health in
Massachusetts; A Massachusetts
Community Health Workers Survey
Report. Boston, MA: Division of
Primary Care and Health Access
Centers for Community Health,
Massachusetts Department of Public
Health, 2005.
Bates, Benjamin R. “The (In) Appropriateness
of the WAR Metaphor in Response to
SARS-CoV-2: A Rapid Analysis of
Donald J. Trump’s Rhetoric.” Frontiers
in Communication 5 (2020): 50.
Bishop, Christine, et al. “Implementing a
Natural Helper Pay Health Advisor
Program: Lessons Learned from
Unplanned Events.” Journal of Health
Promotion Practice 3, no. 2 (2002):
233–244.
Dieleman, Marjolein, Pham Viet Cuong, Le
Anh, and Tam Martineau. “Identifying
Factors for Job Motivation of Rural
Health Workers in North Viet Nam.”
Human Resource for Health 1, no. 10
(May 2003). Accessed October 18,
2024.
Flusberg, Stephen J., T. Matlock, and P. H.
Thibodeau. “War Metaphors in Public
Discourse.” Metaphor and Symbol 33,
no. 1 (2018): 1–18.
Franco, Lynne M., Sara Bennett, and Ruth
Kanfer. “Health Sector Reform and
Public Sector Health Worker
Motivation.” Social Science & Medicine
54, no. 8 (2002): 1255–1266.
Ghosh, Ananya. “India’s All-Women Frontline
Defense Against COVID-19 Fight for
Fair Pay.” Open Democracy Feature,
2021.
Glenton, Claire, Christopher J. Colvin, Bente
Carlsen, Alison Swartz, Simon Lewin,
Jane Noyes, and et al. “Barriers and
Facilitators to Implementing Lay
Health Worker Programs to Improve
Maternal and Child Health Access: A
Qualitative Evidence Synthesis.”
Cochrane Database of Systematic
Reviews 10 (2013): CD010414.
International Institute for Population Sciences (IIPS) and Ministry of Health and
Family Welfare, Government of India.
National Family Health Survey (NFHS
5), 2019-21. Mumbai: IIPS, 2021.
Javanparast, Sepideh, John Coveney, and
Utpal Saikia. “A Qualitative Study
Explores Health Stakeholders’
Perceptions
of
Providing
Comprehensive Primary Health Care
to Address Childhood Malnutrition in
Iran.” BMC Health Services Research
9, no. 36, 2009.
Joshi, R. S., and M. George. “Healthcare
Through Community Participation:
Role of ASHAs.” Economic and Political
Weekly 47, no. 10 (2012): 70–76.
Khan, Mohammad Haroon, et al. “Assessment
of Knowledge, Attitude, and Skills of
Lady Health Workers.” Gomal Journal
of Medical Sciences 4, no. 2, 2006.
Mahyavanshi, K. D., M. G. Patel, et al. “A
Cross-Sectional Study of the
Knowledge, Attitude, and Practice of
ASHA Workers Regarding Child Health
(Under Five Years of Age) in
Surendranagar District.” Healthline 7,
no. 2 (2011): 50–55.
Ministry of Health and Family Welfare,
Government of India. Mission
Indradhanush. 2019.
Ministry of Health and Family Welfare,
Government of India. National Health
Mission. 2022.
Mishra, Arima. “‘Trust and Teamwork Matter’:
Community Health Workers’
Experiences in Integrated Service
Delivery in India.” Global Public Health
9, no. 8 (2014): 960–974.
Mundhra, D. D. “Intrinsic Motivational Canvas
in the Indian Service Sector: An
Empirical Study.” The Journal of
Business Perspective 14, no. 4 (2010):
275–285.
Nair, H. V., N. Sasidharan, A. Sreedevi, et al.
“Role and Function of Frontline Health
Workers During the COVID-19
Pandemic in a Rural Health Center in
Kerala: A Qualitative Study.” Cureus
16, no. 9 (2024): e69128.
Nanda, Priya, T. N. Lewis, P. Das, and S.
Krishnan. “From the Frontlines to
Center Stage: Resilience of Frontline
Health Workers in COVID-19.” Sexual
and Reproductive Health Matters,
2020.
Nandi, Sulakshana, and Helen Schneider.
“Using an Equity-Based Framework
for Evaluating Publicly Funded Health
Insurance Programs as an Instrument
of UHC in Chhattisgarh State, India.”
Health Research Policy and Systems
18 (2020): 50.
National Family Health Survey (NFHS-4),
2015-16: International Institute for
Population Sciences (IIPS) and
Ministry of Health and Family Welfare,
Government of India. Mumbai: IIPS,
2017.
National Rural Health Mission. Guidelines for
Community Processes. Nirman
Bhavan: Ministry of Health and Family
Welfare, 2013.
Office of the Registrar General, India. Sample
Registration System (SRS) Bulletin.
Ministry of Home Affairs, Government
of India, 2022.
Pfrimer, Matheus H., and R. Barbosa. “Brazil’s
War on COVID-19: Crisis, Not
Conflict—Doctors, Not Generals.”
Dialogues in Human Geography 10, no.
2 (2020): 137–140.
Policy Brief. “The Role of Gender Bias in
Gender-Based Violence in India.”
University of Huddersfield, 2018.
Sarin, Enisha, and Sharon S. Lunsford. “How
Female Community Health Workers
Navigate Work Challenges and Why
There Are Still Gaps in Their
Performance: A Look at Female
Community Health Workers in Maternal and Child Health in Two
Indian Districts Through a Reciprocal
Determinism Framework.” Human
Resources for Health 15, no. 44, 2017.
Scott, Kerry, and Sabina Shanker. 2010. “Tying
Their Hands? Institutional Obstacles to
the Success of the ASHA Community
Health Worker Program in Rural North
India.” Aids Care – Psychological and
Socio-Medical Aspects of Aids/HIV 22,
no. 12: 1606–1612.
Scott, Kerry, Abhijit S. George, and R. R. Ved.
2019. “Taking Stock of 10 Years of
Published Research on the ASHA
Programme: Examining India’s
National Community Health Worker
Programme from a Health Systems
Perspective.” Health Research Policy
and Systems 17, no. 1: 1–17.
Taylor, Nik, and Ben Lohmeyer. “War, Heroes,
and Sacrifice.” Critical Sociology,
2020.
USAID India. Accredited Social Health Activist
Plus Scheme. 2008.
Ved, R., Kerry Scott, and Abhijit S. George.
“How Are Gender Inequalities Facing
India’s One Million ASHAs Being
Addressed?” Human Resources for
Health 17, no. 1 (2019): 1–15.
Vir, Sheila C. Child, Adolescent and Woman
Nutrition in India – Public Policies,
Programmes, and Progress.
Routledge, 2023.
Vroom, Victor H. “Expectancy Model, and
Work-Related Criteria: A Meta
Analysis.” Journal of Applied
Psychology 81, no. 5, 1996.
Walt, Gill. “CHWs: Are National Programmes
in Crisis?” Health Policy & Planning 31,
no. 1 (1989): 1–21.
World Health Organisation. Declaration of
Alma Ata. 1978.
Conflict of interest: None
Role of funding source: None


