Indian Journal of Health Social Work
(UGC Care List Journal)
EFFICACY OF SINGLE SESSION WORKSHOP USING PRINCIPLES OF
ACT IN PROMOTING PSYCHOLOGICAL HELP-SEEKING IN HIGHER
EDUCATION SETTINGS: A PRELIMINARY SURVEY
Vikas Kumar1 & Shuvabrata Poddar2
1PhD Research Scholar, Department of Applied Psychology, Kazi Nazrul University, Asansol, and
Assistant Professor, Amity Institute of Clinical Psychology, Amity University, Patna. 2Assistant
Professor, Department of Applied Psychology, Kazi Nazrul University, Asansol.
Correspondence: Vikas Kumar, e-mail: ku.vikasbhu@gmail.com
ABSTRACT
Background: The reluctance of higher education students to seek psychological care, despite
rising mental health concerns, highlights the importance of brief and effective interventions.
This study investigates the efficacy of a single-session Acceptance and Commitment Therapy
(ACT) intervention in improving psychological help-seeking behaviour among college students.
Methods & Materials: A sample of 30 students took part in a pre-post experimental design,
with help-seeking attitudes measured using the Attitudes Toward Seeking Professional
Psychological Help Scale (ATSPPH-SF). Results: The findings demonstrated a statistically
significant increase in attitudes toward help-seeking following intervention, showing the potential
of ACT as a brief, effective method. Conclusion: These findings have significance for campus
mental health outreach and the incorporation of ACT into prevention initiatives.
Keywords: Single-Session Intervention, Acceptance and Commitment Therapy, Help-Seeking
Behaviour, Higher Education, Students’ Mental Health.
INTRODUCTION
Mental health concerns among higher
education students are on the rise, with a
significant portion of students experiencing
stress, anxiety, depression, and adjustment
difficulties (Hunt & Eisenberg, 2010). Despite
the increasing prevalence of psychological
issues, a large number of students do not
actively seek professional psychological help.
Barriers such as stigma, lack of awareness,
cultural misconceptions, and negative
attitudes toward counselling contribute to this
help-seeking gap (Rickwood et al., 2007;
Eisenberg, Speer, & Hunt, 2012).
In recent years, researchers have worked to
understand and remove these barriers, with
a focus on designing brief, accessible, and
effective psychological interventions that
encourage people to seek mental health help.
Acceptance and Commitment Therapy (ACT)
is one strategy that has produced encouraging
outcomes. Hayes, Strosahl, and Wilson (1999)
developed ACT, a third-wave behavioural
intervention that stresses psychological
flexibility by encouraging people to accept their
internal experiences while doing meaningful,
value-driven behaviours. ACT consists of six key processes: cognitive defusion,
acceptance, touch with the present moment,
self-observation, values, and committed
action (Hayes et al., 2006). Unlike traditional
cognitive-behavioural therapy (CBT), which
focuses on changing the content of thoughts,
ACT promotes a new relationship with
thoughts and feelings—allowing individuals to
engage in valued behaviours even in the
presence of discomfort. This makes it
particularly suitable for individuals
experiencing internal conflicts, avoidance, or
fear around psychological support and stigma.
Research suggests that ACT can effectively
treat depression, anxiety, and stress (Powers
et al., 2009; Öst, 2014). Furthermore, new
research has looked into the impact of brief
ACT interventions, including single-session
formats, on particular objectives like stress
reduction, self-stigma reduction, and
psychological flexibility (Levin et al., 2017).
However, its use in directly influencing help
seeking behaviour among university students
remains relatively unexplored, particularly in
the Indian setting. According to research,
young adults, particularly those in college,
frequently struggle to recognize their mental
health issues and seek prompt professional
help (Gulliver, Griffiths, & Christensen, 2010).
Attitudes toward psychological help-seeking
play a pivotal role in this behaviour, where
negative beliefs or internalized stigma reduce
the likelihood of accessing available services
(Corrigan, 2004). In a meta-analytic review,
Vogel, Wester, and Larson (2007) found that
self-stigma was negatively associated with
help-seeking attitudes and intentions. Such
internal barriers are prevalent among Indian
students as well, where cultural expectations
and lack of psychological awareness further
complicate help-seeking efforts (Sharma &
Reddy, 2015). Intervention strategies aimed
at improving help-seeking behaviours have
traditionally involved awareness programs,
psychoeducation, or stigma reduction
campaigns (Yorgason, Linville, & Zitzman,
2008). However, these approaches often
require multiple sessions or institutional
commitment. Hence, brief interventions that
can be implemented in a single session and
still demonstrate efficacy are especially
valuable.
The effectiveness of single-session
interventions (SSIs) in both clinical and non
clinical populations has drawn attention due
to their focused and efficient effects (Schleider
& Weisz, 2017). According to Levin et al.
(2014) and Bricker et al. (2013), ACT-based
SSIs have been shown to be successful in
l owering experiential avoidance and
enhancing psychological flexibility and self
compassion. These are important processes
to overcome internal resistance to asking for
help. Levin et al. (2017) showed that even a
one-hour ACT-based intervention significantly
reduced stigma around mental health and
increased college students’ receptivity to
therapy. By focusing on acceptance and values
clarification, ACT helps people rewrite their
inner stories and create space for self-care
related actions, such as asking for help.
Studies explicitly examining ACT’s effect on
help-seeking attitudes are still scarce despite
these encouraging results, especially in
academic contexts with limited resources or
high levels of stigma in developing nations.
In order to fill this gap, this study investigates
i f ACT, even for just one session, can
i nfluence students’ attitudes toward
requesting assistance.
The underutilization of psychological services
by students despite increasing mental health
concerns presents a serious challenge for
educational institutions and mental health
professionals. According to Eisenberg et al.
(2012), over 60% of college students
experiencing mental health issues do not seek
any form of professional support. In India, the
challenge is compounded by cultural norms,
stigma, and a lack of mental health infrastructure in academic settings. Many
students hesitate to seek help due to
internalized shame, fear of judgment, or
belief that their problems should be managed
independently (Sahoo & Khess, 2010). Given
these barriers, there is an urgent need to test
and implement evidence-based, low-cost, and
scalable interventions that can be delivered
within the campus environment. ACT, with its
emphasis on value-driven behaviour and
acceptance, is particularly well-suited to
target psychological inflexibility—one of the
key predictors of avoidance and inaction in
mental health seeking (Hayes et al., 2006).
Furthermore, because students may be unable
to attend therapy because of time constraints,
conflicting academic priorities, or early
resistance to multi-session treatment, single
session models are well-suited for the higher
education setting. By reducing psychological
resistance and encouraging a more positive
attitude toward therapy, a successful one
session ACT intervention may serve as a
“gateway experience” into professional help
seeking behaviour. Therefore, by examining
the early efficacy of a single-session ACT
based intervention in altering students’
attitudes toward seeking help, the current
study seeks to close a substantial research
and practice gap. Additionally, keep in mind
that single-session models work best in higher
education settings when students may initially
be resistant to multi-session therapy or have
time constraints or conflicting academic
obligations. Because it lowers psychological
resistance and fosters more adaptable
attitudes toward therapy, a successful one
session ACT intervention could be used as a
first step toward getting help. In light of this,
this study closes a significant research and
practice gap by evaluating the initial efficacy
of a one-session ACT-based intervention in
altering students’ attitudes toward seeking
help.
METHODOLOGY
Participants
The study was conducted with a sample of 30
higher education students (n = 30) enrolled
in undergraduate and postgraduate courses
across various disciplines at universities in
India. Participants were selected using
purposive sampling. The inclusion criteria
required participants to be between 18 and
25 years old and to have not received any
form of psychological intervention in the last
six months. Those with a diagnosed
psychiatric condition were excluded.
Design
A pre-post single-group experimental design
was used to evaluate the effectiveness of a
Single-Session Acceptance and Commitment
Therapy (ACT) intervention on psychological
help-seeking behaviour.
TOOLS USED
1. Acceptance and Action Questionnaire – II
(AAQ-II): The AAQ-II is a 7-item self
report instrument developed by Bond et
al. (2011) to assess psychological
inflexibility or experiential avoidance. Each
item is rated on a 7-point Likert scale
ranging from 1 (“never true”) to 7
(“always true”). Higher scores indicate
greater psychological inflexibility. The
AAQ-II has demonstrated good internal
consistency (á = .84) and test-retest
reliability (r = .81) (Bond et al., 2011).
2. Self-Stigma of Seeking Help Scale (SSOSH): The SSOSH is a 10-item scale designed by Vogel et al. (2006) to assess the degree to which individuals believe they would be devalued if they sought psychological help. Items are rated on a 5-point Likert scale from 1 (“strongly disagree”) to 5 (“strongly agree”). Higher scores suggest higher levels of self stigma. The scale has shown adequate internal consistency (á = .86).
3. Attitudes Toward Seeking Professional Psychological Help Scale – Short Form (ATSPPH-SF): This is a 10-item scale developed by Fischer and Farina (1995) to measure general attitudes toward seeking psychological help. It uses a 4 point Likert scale ranging from 0 (“disagree”) to 3 (“agree”). Higher scores represent more positive attitudes. The ATSPPH-SF has demonstrated acceptable internal reliability (á = .77) and validity across different populations.
2. Self-Stigma of Seeking Help Scale (SSOSH): The SSOSH is a 10-item scale designed by Vogel et al. (2006) to assess the degree to which individuals believe they would be devalued if they sought psychological help. Items are rated on a 5-point Likert scale from 1 (“strongly disagree”) to 5 (“strongly agree”). Higher scores suggest higher levels of self stigma. The scale has shown adequate internal consistency (á = .86).
3. Attitudes Toward Seeking Professional Psychological Help Scale – Short Form (ATSPPH-SF): This is a 10-item scale developed by Fischer and Farina (1995) to measure general attitudes toward seeking psychological help. It uses a 4 point Likert scale ranging from 0 (“disagree”) to 3 (“agree”). Higher scores represent more positive attitudes. The ATSPPH-SF has demonstrated acceptable internal reliability (á = .77) and validity across different populations.
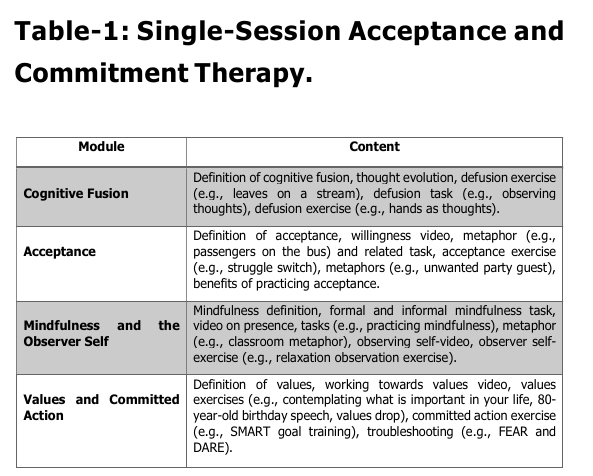
INTERVENTION
Single-Session Acceptance and Commitment
Therapy (SSACT) based intervention was
applied with students as a therapeutic
module, adapted from Thomas, K. (2021) ‘s
A One-Session, Brief Acceptance and
Commitment Therapy Workshop. The module
has been adopted for the current study.
However, few therapeutic techniques had been
tailored to meet their need, and a better
understanding of the students was needed to
meet the treatment efficacy. This adapted and
culturally relevant therapeutic module has
been approved by the university ethics
committee. The details of the Single-Session
Acceptance and Commitment Therapy
Workshop are presented in Table 1.
PROCEDURE
Participants were given informed permission
and instructed on the study’s aims. Three
standardized self-report measures were used
to conduct the baseline assessment: the
Acceptance and Action Questionnaire – II
(AAQ-II), the Self-Stigma of Seeking Help
Scale (SSOSH), and the Attitudes Toward
Seeking Professional Psychological Help
Short Form. Following that, participants
received a 90-minute structured single
session ACT intervention that emphasized
cognitive defusion, acceptance, value
clarification, and committed action. A week
later, post-intervention assessments utilizing
the same three measures were done.
RESULTS
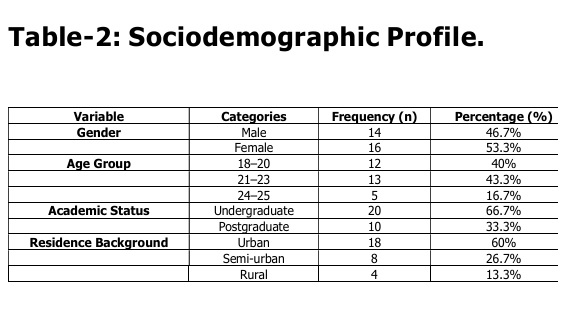
Table-2: explained sample included 16
females (53.3%) and 14 males (46.7%), with
a mean age of 21.4 years (SD = 2.01). The
majority of participants were from urban
backgrounds (60%), while the rest were from
semi-urban (26.7%) and rural (13.3%) areas.
Academic levels included undergraduate
(66.7%) and postgraduate (33.3%) students.
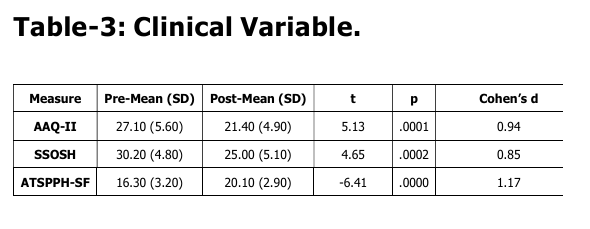
The results revealed statistically significant
differences in the pre-and post-intervention
scores for all three measures:
1. Psychological Inflexibility (AAQ-II):
Scores significantly decreased post intervention (t(29) = 5.13, p < .001), i ndicating improved psychological flexibility. A large effect size (Cohen’s d = 0.94) suggests the ACT session had a substantial impact.
Scores significantly decreased post intervention (t(29) = 5.13, p < .001), i ndicating improved psychological flexibility. A large effect size (Cohen’s d = 0.94) suggests the ACT session had a substantial impact.
2. Self-Stigma (SSOSH):
Participants showed a significant reduction in self stigma (t(29) = 4.65, p < .001). The effect size (d = 0.85) indicates a substantial change in perception toward stigma about help-seeking.
Participants showed a significant reduction in self stigma (t(29) = 4.65, p < .001). The effect size (d = 0.85) indicates a substantial change in perception toward stigma about help-seeking.
3. Attitudes Toward Help-Seeking
(ATSPPH-SF):
Scores significantly increased (t(29) = -6.41, p < .001), reflecting improved attitudes toward seeking professional help. The very large effect size (d = 1.17) highlights the intervention’s robust impact.
Scores significantly increased (t(29) = -6.41, p < .001), reflecting improved attitudes toward seeking professional help. The very large effect size (d = 1.17) highlights the intervention’s robust impact.
DISCUSSION
The present study aimed to evaluate the
effectiveness of a single-session Acceptance
and Commitment Therapy (ACT) intervention
in increasing psychological help-seeking
behaviour among higher education students.
This work was motivated by growing concerns
about poor mental health care utilization rates
among college students despite rising
psychological discomfort (Eisenberg et al.,
2012). The study’s findings give early
evidence that even a brief ACT session can
drastically change students’ attitudes toward
obtaining professional psychological
treatment.
The findings revealed a statistically significant
change in post-intervention ratings on the
Attitudes Toward Seeking Professional
Psychological Help – Short Form (ATSPPH-SF),
i ndicating more positive help-seeking
attitudes following the ACT session. The pre
to post-intervention difference was associated
with a substantial effect size (Cohen’s d =
1.14), indicating both statistical and practical
importance. These findings are consistent
with previous research demonstrating the
effectiveness of ACT in reducing psychological
avoidance and boosting readiness to seek help
(Levin et al., 2016; Roush et al., 2018). This
study expands on existing literature by using
ACT in a single-session format, which has
previously been proven to be helpful in
j uvenile populations for a variety of
psychological disorders (Schleider & Weisz,
2017). The current findings align with the
notion that psychological flexibility—ACT’s
central mechanism—may play a critical role
in changing maladaptive attitudes toward
professional help-seeking.
Psychological Flexibility and Help-Seeking
Behavior
One of the fundamental concepts of ACT is to
improve psychological flexibility, which refers
to the ability to be open to new experiences,
stay present, and act on personal ideals
(Hayes et al., 2006). In the context of
psychological help-seeking, this flexibility
enables people to face the unpleasantness
that comes with seeking help (e.g., stigma,
self-doubt) and commit to behaviours that
promote personal well-being. Previous studies
have demonstrated that more psychological
flexibility is associated with more positive
attitudes about mental health care (Masuda
et al., 2012). In the present study, methods
l ike values clarification, defusion, and
mindfulness were probably crucial in fostering
acceptance of mental health needs and
combating internalized stigma. Through the
use of ACT metaphors, such as “Passengers
on the Bus” or “Tug-of-War with a Monster,”
students who might ordinarily view asking for help as a sign of weakness may be able to
shift their viewpoint and break free from these
damaging narratives. A mental shift brought
about by these hands-on activities can make
people more receptive to receiving support
services.
Role of Stigma in Help-Seeking Barriers
Stigma continues to be one of the most
significant barriers to student mental health
service utilization (Corrigan, 2004). ACT
addresses stigma by increasing acceptance of
stigmatizing beliefs and diminishing their
behavioural influence rather than aiming to
erase them. This method differs from
cognitive-behavioural models in that it focuses
on the process of defusion rather than the
content of stigmatizing beliefs (Hayes et al.,
1999). The current study’s excellent findings
indicate that even in a brief intervention
format, ACT can successfully reduce the
functional impact of stigma on help-seeking
behaviour. By reframing mental health support
as a values-based action rather than a sign
of personal inadequacy, students may become
more inclined to seek help, particularly when
guided by the principle of living a meaningful
life.
Effectiveness of Single-Session Interventions
Utilizing a single-session approach, which is
scalable and resource-efficient, was one
noteworthy feature of the study. Although
multi-session therapies have historically been
the standard in clinical psychology, new
studies have shown the benefits of brief and
ultra-brief interventions, especially for
populations that are reluctant to commit to
longer-term therapy or have time constraints
(Schleider & Weisz, 2016). Key therapeutic
components were crammed into a 90-minute
ACT session, which was intended to be
intense and highly experiential in the current
study. Although brief, the intervention resulted
in a notable change in attitudes, indicating
that content quality and relevance may be
more important than duration, especially in
preventive or attitudinal treatments. This
finding is crucial in higher education settings
since counselling clinics are frequently
underfunded and overburdened (Gallagher,
2014). Implementing brief, ACT-informed
workshops could be a viable first-line method
to enhance psychological openness among
students, thereby increasing the adoption of
additional therapies as needed.
Implications for Practice
The present findings carry several practical
implications:
1. The intervention is cost-effective and needs minimal resources, making it suitable for widespread implementation across academic institutions.
2. ACT can help improve clinical therapy and mental wellness. As a result, the intervention concentrating on attitudes has the potential to improve the early detection and intervention processes.
3. ACT is adjustable and may be adjusted to different groups based on cultural and gender factors, making it incredibly versatile.
4. Non-clinical practitioners, such as academic counsellors or peer mentors, can effectively apply ACT-based therapies with proper training and supervision, expanding their reach.
5. Digitization aligns well with the ACT paradigm. Previous research (Levin et al., 2014) has demonstrated that online delivery of ACT modules improves availability for students who are unwilling to attend face-to-face sessions.
1. The intervention is cost-effective and needs minimal resources, making it suitable for widespread implementation across academic institutions.
2. ACT can help improve clinical therapy and mental wellness. As a result, the intervention concentrating on attitudes has the potential to improve the early detection and intervention processes.
3. ACT is adjustable and may be adjusted to different groups based on cultural and gender factors, making it incredibly versatile.
4. Non-clinical practitioners, such as academic counsellors or peer mentors, can effectively apply ACT-based therapies with proper training and supervision, expanding their reach.
5. Digitization aligns well with the ACT paradigm. Previous research (Levin et al., 2014) has demonstrated that online delivery of ACT modules improves availability for students who are unwilling to attend face-to-face sessions.
Limitations
While the study offers valuable preliminary
i nsights, several limitations must be
acknowledged:
1. With only 30 participants, the study’s findings cannot be generalized. Larger sample sizes would provide better statistical power.
2. The absence of a control or comparison group prevents causal inference. A randomized controlled design would i mprove internal validity in future research.
3. Attitudes were assessed shortly after the intervention. Longitudinal research would be required to assess whether improved attitudes may be converted into actual help-seeking behaviour, as well as whether such an effect is long-lasting.
4. The use of self-report measures, such as the ATSPPH-SF, may result in social desirability or response bias. Accepting behavioural evidence of help-seeking or follow-up usage data from the university counselling service may provide methodological enhancements in future research.
1. With only 30 participants, the study’s findings cannot be generalized. Larger sample sizes would provide better statistical power.
2. The absence of a control or comparison group prevents causal inference. A randomized controlled design would i mprove internal validity in future research.
3. Attitudes were assessed shortly after the intervention. Longitudinal research would be required to assess whether improved attitudes may be converted into actual help-seeking behaviour, as well as whether such an effect is long-lasting.
4. The use of self-report measures, such as the ATSPPH-SF, may result in social desirability or response bias. Accepting behavioural evidence of help-seeking or follow-up usage data from the university counselling service may provide methodological enhancements in future research.
Recommendations for Future Research
1. Comparing ACT against control groups or
other brief therapies, such as
psychoeducation or motivational
interviewing, can provide more conclusive
evidence of success.
2. Tracking help-seeking behaviours for 3 to 6 months after intervention can assess the long-term impact of attitudinal change.
3. To further understand how ACT affects help-seeking behaviour, it’s important to investigate if psychological flexibility or stigma plays a role.
4. Adapting ACT to varied student demographics, particularly those with collectivistic ideals, can increase its acceptability and effectiveness.
5. Collaborating with student mental health groups or peer counsellors can increase reach and engagement, especially for students who are unsure about formal psychological services.
2. Tracking help-seeking behaviours for 3 to 6 months after intervention can assess the long-term impact of attitudinal change.
3. To further understand how ACT affects help-seeking behaviour, it’s important to investigate if psychological flexibility or stigma plays a role.
4. Adapting ACT to varied student demographics, particularly those with collectivistic ideals, can increase its acceptability and effectiveness.
5. Collaborating with student mental health groups or peer counsellors can increase reach and engagement, especially for students who are unsure about formal psychological services.
CONCLUSION
The current study provides hopeful evidence
t hat one session of Acceptance and
Commitment Therapy (ACT) can positively
i nfluence higher education students’
psychological help-seeking attitudes. Though
the intervention was brief, the impact on
students’ willingness to seek professional
psychiatric care was significant and
important. Given the critical need to address
mental health issues in higher education
settings, time-limited, low-threshold, and
scalable therapies like ACT have enormous
potential. The ACT process works by
i ncreasing psychological flexibility,
normalizing experiencing discomfort, and
beginning action that aligns with personal
beliefs. As a result, it could play an important
role in lowering obstacles to mental health
treatment. Although further research is
required to analyze and expand on these
preliminary findings, the therapeutic
implications are promising and practical.
REFERENCES
Bond, F. W., Hayes, S. C., Baer, R. A.,
Carpenter, K. M., Guenole, N., Orcutt,
H. K., … & Zettle, R. D. (2011).
Preliminary psychometric properties of
t he Acceptance and Action
Questionnaire–II: A revised measure
of psychological inflexibility and
experiential avoidance. Behavior
Therapy, 42(4), 676–688. https://
doi.org/10.1016/j.beth.2011.03.007
Bricker, J. B., Wyszynski, C. M., Comstock, B.
A., & Heffner, J. L. (2013). Pilot
randomized controlled trial of web
based acceptance and commitment
therapy for smoking cessation.
Nicotine & Tobacco Research, 15(10),
1756–1764. https://doi.org/10.1093/ ntr/ntt035
Corrigan, P. (2004). How stigma interferes
with mental health care. American
Psychologist, 59(7), 614–625. https:/
/doi.org/10.1037/0003-066X.59.7.614
Corrigan, P. (2004). How stigma interferes
with mental health care. American
Psychologist, 59(7), 614–625. https:/
/doi.org/10.1037/0003-066X.59.7.614
Eisenberg, D., Hunt, J., & Speer, N. (2012).
Help seeking for mental health on
college campuses: Review of
evidence and next steps for research
and practice. Harvard Review of
Psychiatry, 20(4), 222–232. https://
d o i . o r g / 1 0 . 3 1 0 9 /
10673229.2012.712839
Eisenberg, D., Speer, N., & Hunt, J. B. (2012).
Attitudes and beliefs about treatment
among college students with
untreated mental health problems.
Psychiatric Services, 63(7), 711–713.
h t t p s : / / d o i . o r g / 1 0 . 1 1 76 /
appi.ps.201100250
Fischer, E. H., & Farina, A. (1995). Attitudes
t oward seeking professional
psychological help: A shortened form
and considerations for research.
Journal of College Student
Development, 36(4), 368–373.
Gallagher, R. P. (2014). National survey of
college counseling centers 2014.
American College Counseling
Association.
Gulliver, A., Griffiths, K. M., & Christensen, H.
(2010). Perceived barriers and
facilitators to mental health help
seeking in young people: A systematic
review. BMC Psychiatry, 10, 113.
https://doi.org/10.1186/1471-244X
10-113
Hayes, S. C., Luoma, J. B., Bond, F. W.,
Masuda, A., & Lillis, J. (2006).
Acceptance and commitment therapy:
Model, processes and outcomes.
Behaviour Research and Therapy,
44(1), 1–25. https://doi.org/10.1016/
j.brat.2005.06.006
Hayes, S. C., Luoma, J. B., Bond, F. W.,
Masuda, A., & Lillis, J. (2006).
Acceptance and commitment therapy:
Model, processes and outcomes.
Behaviour Research and Therapy,
44(1), 1–25. https://doi.org/10.1016/
j.brat.2005.06.006
Hayes, S. C., Strosahl, K. D., & Wilson, K. G.
(1999). Acceptance and commitment
therapy: An experiential approach to
behavior change. Guilford Press.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G.
(1999). Acceptance and Commitment
Therapy: An experiential approach to
behavior change. Guilford Press.
Hunt, J., & Eisenberg, D. (2010). Mental health
problems and help-seeking behavior
among college students. Journal of
Adolescent Health, 46(1), 3–10.
h t t p s : / / d o i . o r g / 1 0 . 1 0 16 /
j.jadohealth.2009.08.008
Levin, M. E., Haeger, J., Pierce, B. G., & Cruz,
R. A. (2017). Evaluating an
acceptance and commitment therapy
workshop for college students: A
randomized controlled trial. Cognitive
Behaviour Therapy, 46(1), 1–20.
h t t p s : / / d o i . o r g / 1 0 . 1 0 80 /
16506073.2016.1214293
Levin, M. E., Krafft, J., Pistorello, J., Seeley,
J. R., & Hayes, S. C. (2017). Evaluating
an acceptance and commitment
t herapy workshop for college
students: A randomized controlled
trial. Cognitive Behaviour Therapy,
46(1), 1–20. https://doi.org/10.1080/
16506073.2016.1214293
Levin, M. E., Pistorello, J., Seeley, J. R., &
Hayes, S. C. (2014). Testing the
effects of a web-based acceptance
and commitment therapy intervention
for mental health stigma. Behavior Modification, 38(6), 791–813. https:/
/doi.org/10.1177/0145445514524880
Masuda, A., Anderson, P. L., & Sheehan, S. T.
(2009). Cognitive defusion and self
relevant negative thoughts: Examining
the impact of a ninety year old
technique. Behaviour Research and
Therapy, 47(7), 565–573. https://
doi.org/10.1016/j.brat.2009.03.003
Öst, L. G. (2014). The efficacy of Acceptance
and Commitment Therapy: An updated
systematic review and meta-analysis.
Behaviour Research and Therapy, 61,
105–121. https://doi.org/10.1016/
j.brat.2014.07.018
Powers, M. B., Zum Vörde Sive Vörding, M.
B., & Emmelkamp, P. M. (2009).
Acceptance and Commitment
Therapy: A meta-analytic review.
Psychotherapy and Psychosomatics,
78(2), 73–80. https://doi.org/
10.1159/000190790
Rickwood, D., Deane, F. P., Wilson, C. J., &
Ciarrochi, J. (2007). Young people’s
help-seeking for mental health
problems. Australian e-Journal for the
Advancement of Mental Health, 4(3),
218–251.
Roush, S. E., Brown, S. L., & Morrow, S. L.
(2018).
College
students’
psychological help-seeking intentions
and behavior: An application of the
Theory of Planned Behavior. Journal
of American College Health, 66(5),
421–429. https://doi.org/10.1080/
07448481.2018.1440570
Sahoo, S., & Khess, C. R. J. (2010).
Understanding stigma and its impact
on mental health. Mental Health: An
Indian Perspective, 217–225.
Schleider, J. L., & Weisz, J. R. (2016).
Reducing risk for anxiety and
depression in adolescents: Effects of
a single-session intervention teaching
that personality can change. Behaviour
Research and Therapy, 87, 170–181.
h t t p s : / / d o i . o r g / 1 0 . 1 0 16 /
j.brat.2016.09.011
Schleider, J. L., & Weisz, J. R. (2017). Little
treatments, promising effects? Meta
analysis
of
single-session
interventions for youth psychiatric
problems. Journal of the American
Academy of Child and Adolescent
Psychiatry, 56(2), 107–115. https://
doi.org/10.1016/j.jaac.2016.11.007
Schleider, J. L., & Weisz, J. R. (2017). Little
treatments, promising effects? Meta
analysis
of
single-session
interventions for youth psychiatric
problems. Journal of the American
Academy of Child and Adolescent
Psychiatry, 56(2), 107–115.
Sharma, M., & Reddy, S. (2015). Barriers to
mental health service utilization
among students in India: A systematic
review. International Journal of
Culture and Mental Health, 8(2), 120
136. https://doi.org/10.1080/
17542863.2014.892531
Twohig, M. P., & Levin, M. E. (2017).
Acceptance and Commitment Therapy
as a treatment for anxiety and
depression: A review. Psychiatric
Clinics of North America, 40(4), 751
770. https://doi.org/10.1016/
j.psc.2017.08.009
Vogel, D. L., Wade, N. G., & Haake, S. (2006).
Measuring the self-stigma associated
with seeking psychological help.
Journal of Counseling Psychology,
53(3), 325–337. https://doi.org/
10.1037/0022-0167.53.3.325
Vogel, D. L., Wester, S. R., & Larson, L. M.
(2007). Avoidance of counseling:
Psychological factors that inhibit
seeking help. Journal of Counseling &
Development, 85(4), 410–422. https:/
/ d o i . o r g / 1 0. 1 002/j. 1 5 56
6678.2007.tb00609.x Yorgason, J. B., Linville, D., & Zitzman, B.
(2008). Mental health help-seeking
intentions among college students:
Assessing the role of perceived norms
and stigma. Journal of College Student
Psychotherapy, 22(4), 306–320.
h t t p s : / / d o i . o r g / 1 0 . 1 0 80 /
87568220802397441
Conflict of interest: None
Role of funding source: None


