Background: Obsessive-Compulsive Disorder (OCD) is a chronic and debilitating psychiatric
condition characterized by persistent obsessions and compulsions that significantly impair various
domains of functioning. While much research has focused on symptomatology and treatment
outcomes, there is growing interest in understanding the cognitive-emotional processes that
contribute to functional disability in OCD. Aim: This study explores the relationship between
cognitive emotion regulation strategies and levels of disability in individuals diagnosed with OCD.
Methods: A quantitative, exploratory, and correlational research design was employed to assess
both adaptive and maladaptive emotion regulation strategies and their associations with disability.
Results: Findings from this study are expected to offer insights into how specific emotion regulation
strategies influence daily functioning in individuals with OCD and highlight the potential for
integrating emotion regulation training into therapeutic interventions. Conclusion: The
implications of the results are particularly relevant for mental health professionals in the Indian
context and may aid in the development of more holistic, function-focused treatment approaches.
Keywords:Obsessive-Compulsive Disorder, Emotion Regulation, Functional Disability, IDEAS
Scale, Cognitive Strategies
Obsessive-Compulsive Disorder (OCD) is a
chronic, debilitating neuropsychiatric condition
that significantly impacts an individual’s
quality of life and ability to function across
multiple domains. Characterized by the
presence of obsessions—recurrent and
persistent thoughts, impulses, or images that
are experienced as intrusive and distressing—
and compulsions—repetitive behaviors or
mental acts performed to reduce the distress
associated with obsessions—OCD often leads
to a vicious cycle of anxiety and maladaptive
coping. These symptoms are time-consuming
(typically taking more than an hour per day), ego-dystonic, and are not attributable to the
physiological effects of a substance or another
medical condition (ICD-10, WHO, 1992; DSM
5, APA, 2013). The condition can severely
disrupt an individual’s personal, social,
occupational, and academic functioning,
resulting in a marked decline in overall
psychosocial well-being.
OCD commonly begins in adolescence or early
adulthood and follows a chronic course if left
untreated. It is equally prevalent in both
sexes, although the onset in males tends to
be earlier. The disorder is frequently comorbid
with other psychiatric conditions such as
depression, anxiety disorders, tic disorders,
and body dysmorphic disorder, further
compounding its impact and complicating its
treatment. Despite the availability of evidence
based pharmacological (e.g., SSRIs) and
psychological treatments (e.g., Cognitive
Behavioral Therapy with Exposure and
Response Prevention), many individuals
experience only partial remission or relapse,
underlining the need to investigate other
f actors that contribute to symptom
persistence and functional outcomes.
Epidemiologically, OCD is recognized as a
common psychiatric disorder. According to the
Epidemiological Catchment Area (ECA) study
conducted in the United States, the lifetime
prevalence of OCD ranged from 1.9% to 3.3%
(ECA, 1984). The National Comorbidity Survey
Replication (NCS-R) reported a slightly lower
lifetime prevalence of 2.3% (Kessler et al.,
2005). In global contexts, prevalence
estimates vary: in Iran, it stands at 1.8%, and
in Singapore, at 3%. Studies in India have
also reported prevalence rates between 0.6%
to 3%, depending on the population sampled
and assessment methodology. Importantly, a
significant portion of the population
experiences subclinical obsessive-compulsive
symptoms—manifesting patterns that
resemble OCD but do not meet full diagnostic
criteria. These subthreshold forms can still
lead to distress and functional impairment,
and they may represent a prodromal stage of
the disorder (Weissman et al., 1994). Given
t his spectrum of symptom severity,
understanding the broader implications of OCD
on functioning is critical.
One such domain deserving closer scrutiny is
emotion regulation—the processes by which
individuals influence which emotions they
have, when they have them, and how they
experience and express these emotions
(Gross, 1998). Adaptive emotion regulation
strategies (such as cognitive reappraisal,
positive refocusing, and planning) enable
individuals to manage negative affect and
cope effectively with life’s stressors. In
contrast, maladaptive strategies (such as
rumination, self-blame, catastrophizing, and
suppression) have been linked to a host of
psychological difficulties, including anxiety and
mood disorders (Garnefski & Kraaij, 2006;
Nolen-Hoeksema et al., 2008). In OCD,
emotion dysregulation plays a particularly
central role, as individuals often report intense
feelings of guilt, fear, and distress in response
to intrusive thoughts, which they then attempt
to neutralize through compulsive behaviors.
Over time, reliance on maladaptive strategies
not only perpetuates the obsessive-compulsive
cycle but also undermines self-efficacy and
resilience, thereby aggravating functional
disability.
The association between emotion regulation
and clinical outcomes in OCD has received
increasing empirical attention in recent years.
Studies suggest that difficulties in emotion
regulation are associated with greater
symptom severity, poorer insight, and
reduced treatment responsiveness in OCD.
However, fewer studies have explicitly
examined the impact of emotion regulation on
functional disability—a key determinant of
long-term prognosis and recovery. Disability,
in the context of mental illness, is defined as
the degree to which symptoms interfere with an individual’s ability to carry out age
appropriate and culturally expected roles and
responsibilities. It is not merely the presence
of symptoms, but the extent of functional
impairment, that determines the overall
burden of illness.
In the Indian context, the Indian Disability
Evaluation and Assessment Scale (IDEAS)—
developed by the Rehabilitation Committee of
the Indian Psychiatric Society and endorsed
by the Government of India—is used to assess
disability in individuals with mental illness.
The scale evaluates functioning across four
domains: self-care, interpersonal activities,
communication and understanding, and work.
Each domain is rated on a 5-point scale from
0 (no disability) to 4 (profound disability), and
the total score reflects the level of disability,
categorized as mild (score 1–6), moderate
(7–13), severe (14–19), or profound (20 and
above). In cases where the mental illness has
lasted for more than two years, a weightage
of 1.5 times the total score is applied to
account for chronicity. The IDEAS scale is
widely used for certifying disability in clinical
settings and plays a crucial role in accessing
benefits and rehabilitation services under the
Rights of Persons with Disabilities (RPWD)
Act, 2016.
Despite the clear utility of the IDEAS scale and
the known role of emotion regulation in OCD,
limited research has examined how specific
emotion regulation strategies influence the
level of disability in individuals with OCD.
Given that OCD is often associated with high
levels of functional impairment even when
symptom severity appears moderate, it
becomes essential to explore the mediating
or moderating effects of cognitive-emotional
processes. Understanding these associations
can inform more tailored and effective
interventions aimed not just at reducing
symptoms but at improving overall functioning
and quality of life.
Hence, this study aims to explore the patterns
of cognitive emotion regulation strategies and
their relationship with functional disability in
i ndividuals diagnosed with Obsessive
Compulsive Disorder, using the IDEAS scale
as a measure of disability severity. By
identifying specific maladaptive and adaptive
strategies that are linked with higher or lower
levels of disability, the study seeks to provide
empirical evidence for integrating emotion
regulation training into therapeutic programs
for OCD, particularly in the Indian context.
This chapter presents a detailed account of
the methods adopted for the present study,
which seeks to understand the role of
cognitive emotion regulation strategies in
i ndividuals diagnosed with Obsessive
Compulsive Disorder (OCD), and how these
strategies relate to the levels of disability
experienced by them. It provides a
comprehensive explanation of the study
design, aim and objectives, hypothesis,
sampling method, assessment tools,
procedural steps, and ethical considerations
involved.
The current study follows a quantitative,
exploratory, and correlational design. It
explores the relationship between cognitive
emotion regulation strategies and functional
disability in individuals with OCD, helping to
gain deeper insights into the psychological
coping mechanisms of these individuals and
how they may impact everyday functioning.
Aim & Objectives
To examine the cognitive emotion regulation
strategies adopted by individuals with
obsessive-compulsive disorder (OCD) and
their association with the level of disability.To
assess the cognitive emotion regulation
strategies used by individuals with OCD.
1.
To assess the level of disability in
individuals with OCD.
2.
To examine the relationship between
cognitive emotion regulation strategies
and the level of disability in OCD.
The study was conducted on a sample of 30
individuals diagnosed with OCD, as per ICD
10 criteria. The participants were aged
between 20 to 45 years, with a mean age of
31 years. The educational qualification of
participants ranged from 5th standard to
postgraduate level. All participants were
recruited from the Institute of Mental Health
and Hospital (IMHH), Agra, ensuring clinical
validity of diagnosis and setting.
Participants included individuals aged between
20 to 45 years, with a confirmed diagnosis of
Obsessive-Compulsive Disorder as per ICD
10 criteria, who had an education level of at
least 5th standard and provided informed
consent to participate in the study.
Individuals were excluded from the study if
they had a comorbid diagnosis of any other
psychiatric disorder, a family history of severe
mental illness, or an education level below
5th standard.
1. Consent Form
All participants were provided with an
informed consent form outlining the
purpose of the study, voluntary nature
of participation, and confidentiality
assurance.
2. Socio-Demographic Data Sheet
A structured form was used to collect
personal and clinical information
i ncluding age, gender, education,
duration of illness, and treatment
history.
3. Yale-Brown Obsessive Compulsive
Scale-II (Y-BOCS-II)
This widely accepted clinician
administered instrument assesses the
severity of obsessions and compulsions
through a 10-item severity scale and a
comprehensive symptom checklist. Each
item is rated on a scale from 0 to 5,
offering subscale scores for obsessions
and compulsions, and a total severity
score. The Y-BOCS-II has demonstrated
strong reliability and validity in both
clinical and research settings.
4.Cognitive Emotion Regulation
Questionnaire (CERQ)
This self-report tool consists of 36 items
and evaluates nine distinct cognitive
coping strategies employed following
negative life events, including self
blame, acceptance, rumination, positive
refocusing, refocus on planning,
positive reappraisal, putting into
perspective, catastrophizing, and
blaming others. Responses are rated on
a 5-point Likert scale. The CERQ is
reliable and validated, making it suitable
for assessing individual differences in
emotional regulation.
5.Indian Disability Evaluation and
Assessment Scale (IDEAS)
IDEAS, developed by the Rehabilitation
Committee of the Indian Psychiatric
Society and adopted by the Government
of India, assesses psychiatric disability
i n
f our
domains: self-care,
interpersonal activities, communication
and understanding, and work. Each
domain is scored from 0 (no disability)
to 4 (profound disability). A global
disability score is derived, aiding in the
standardized measurement of mental
health-related disability.
Disability, in the context of psychiatric
disorders like OCD, refers to impairments in
various domains of daily functioning. These
include one’s ability to maintain hygiene, communicate effectively, form and sustain
interpersonal relationships, and perform
occupational or educational tasks. The IDEAS
provides a standardized way to quantify these
impairments. Based on the global score,
disability levels can be categorized as:
This classification helps in both clinical
decision-making and in recommending
appropriate psychosocial rehabilitation.
After obtaining institutional ethical clearance,
participants were recruited from the
outpatient and inpatient departments of IMHH,
Agra. Those meeting the inclusion criteria
were approached individually, and the study
was explained to them in detail. Upon
obtaining informed consent, socio
demographic details were recorded.
Subsequently, participants were assessed
using the Y-BOCS-II, CERQ, and IDEAS by
trained clinical psychologists. Standard
administration protocols were followed to
ensure reliability and consistency in data
collection. The ethical clearance was obtained
from the Ethical committee of the institute.
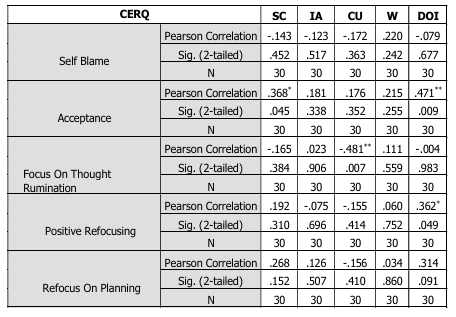
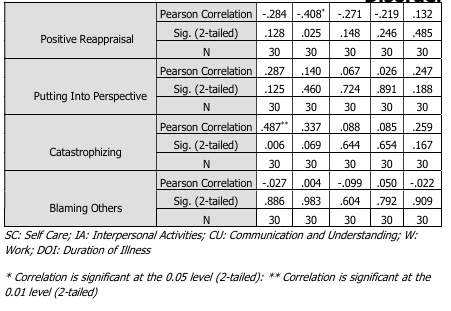
Table 1. Relationship of CERQ with level of
disability.
Table-1: Illustrates the relationship between
various cognitive emotion regulation
strategies (as measured by the CERQ) and
different domains of disability, as well as the
duration of illness. In the self-care domain,
significant correlations at the 0.05 level were
observed for self-blame, acceptance ,
rumination ,positive refocusing, refocus on
planning, positive reappraisal ,and putting into
perspective. Catastrophizing demonstrated a
stronger positive correlation, which was
significant at the 0.01 level. Blaming others
showed a weak negative correlation ,which
was not statistically significant.
In the domain of interpersonal activities,
acceptance ,rumination, positive reappraisal,
putting into perspective ,and catastrophizing
were significantly correlated at the 0.05 level.
In contrast, self-blame, positive refocusing,
refocus on planning ,and blaming others were
not found to be significant.
In the communication and understanding
domain, significant correlations at the 0.05
level were observed for self-blame,
acceptance, positive refocusing, refocus on
planning, and positive reappraisal. Rumination
showed a notable negative correlation,
significant at the 0.01 level. However, putting
into perspective, catastrophizing and blaming
others were not statistically significant.
In the work domain, self-blame, acceptance
and positive reappraisal were significantly
correlated at the 0.05 level. Other subscales such as rumination, positive refocusing,
refocus on planning, putting into perspective,
catastrophizing, and blaming others did not
show significant associations.
With regard to the duration of illness,
significant positive correlations at the 0.05
level were found for positive refocusing ,
refocus on planning, positive reappraisal,
putting into perspective , and catastrophizing.
Acceptance showed a strong positive
correlation, significant at the 0.01 level.
Meanwhile, self-blame and blaming others
were not significantly correlated with the
duration of illness.
The present study aimed to explore the
relationship between cognitive emotion
regulation strategies and various domains of
disability in individuals with obsessive
compulsive disorder.. The findings indicate
that specific cognitive emotion regulation
strategies, as measured by the cognitive
emotion regulation, are significantly
associated with levels of disability across
domains such as self-care, interpersonal
activities, communication and understanding,
and work. Notably, strategies like acceptance,
positive refocusing, refocus on planning,
putting into perspective, and positive
reappraisal were generally associated with
lower levels of disability, suggesting their
adaptive role in psychological adjustment.
Conversely, catastrophizing emerged as a
maladaptive strategy that consistently
correlated with higher levels of disability,
especially in self-care and interpersonal
domains.
The study further found that rumination had
a significant negative association with
communication and understanding, indicating
its detrimental impact on cognitive and social
functioning. Interestingly, blaming others, a
commonly identified maladaptive strategy, did
not significantly correlate with disability in any domain, suggesting that its role may be more
context-dependent or perhaps less influential
i n comparison to internalized emotion
regulation processes like self-blame and
rumination.
The findings also suggest that duration of
illness is positively correlated with the use of
adaptive strategies such as acceptance,
positive refocusing, and refocus on planning,
possibly reflecting the development of coping
mechanisms over time or through therapeutic
interventions.
This study underscores the importance of
cognitive emotion regulation strategies in
influencing disability outcomes in individuals
with mental illness. Adaptive strategies such
as acceptance and positive reappraisal appear
to mitigate disability, while maladaptive ones
l i ke catastrophizing and rumination
exacerbate it. These findings highlight the
potential value of incorporating emotion
regulation training into psychosocial
interventions to enhance functional outcomes.
Several limitations of the present study should
be acknowledged. Firstly, the cross-sectional
design limits the ability to establish causality
between emotion regulation strategies and
disability. Secondly, the study relied on self
report measures, which are subject to biases
such as social desirability and recall errors.
Thirdly, the sample may not be fully
representative of the broader clinical
population, limiting the generalizability of the
findings. Additionally, the study did not
account for the influence of variables such as
medication, severity of illness, or comorbid
conditions, which may have impacted both
emotion regulation and disability levels.
Future research could benefit from
longitudinal designs to better establish the
directionality of relationships between
emotion regulation and disability. It would also
be beneficial to examine the role of clinical variables such as diagnosis type, illness
severity, and treatment history. Furthermore,
intervention studies assessing the impact of
cognitive emotion regulation training on
disability could provide practical insights for
clinical applications. Inclusion of qualitative
approaches may also deepen the
understanding of how individuals perceive and
apply emotion regulation strategies in their
daily lives.
American Psychiatric Association. (2013).
Diagnostic and statistical manual of
mental disorders (5th ed.). Arlington,
VA: American Psychiatric Publishing.
Epidemiologic Catchment Area (ECA) Program.
(1984). The Epidemiologic Catchment
Area (ECA) Program of the National
Institute of Mental Health. Archives of
General Psychiatry, 41(10), 934–941.
h t t p s : / / d o i . o r g / 1 0 . 1 0 0 1 /
archpsyc.1984.01790220016001
Garnefski, N., & Kraaij, V. (2006). Cognitive
emotion regulation questionnaire
development of a short 18-item version
(CERQ-short). Personality and Individual
Differences, 41(6), 1045–1053. https:/
/doi.org/10.1016/j.paid.2006.04.010
Gross, J. J. (1998). The emerging field of
emotion regulation: An integrative
review. Review of General Psychology,
2(3), 271–299. https://doi.org/10.1037/
1089-2680.2.3.271
Indian Psychiatric Society. (2002). Indian
Disability Evaluation and Assessment
Scale (IDEAS): A scale for measuring
and quantifying disability in mental
disorders. Indian Journal of Psychiatry,
44(4), 381–386.
Kessler, R. C., Berglund, P., Demler, O., Jin,
R., Merikangas, K. R., & Walters, E. E.
(2005). Lifetime prevalence and age-of
onset distributions of DSM-IV disorders
in the National Comorbidity Survey
Replication. Archives of General
Psychiatry, 62(6), 593–602. https://
doi.org/10.1001/archpsyc.62.6.593
Nolen-Hoeksema, S., Wisco, B. E., &
Lyubomirsky, S. (2008). Rethinking
rumination.
Perspectives
on
Psychological Science, 3(5), 400–424.
https://doi.org/10.1111/j.1745
6924.2008.00088.x
Weissman, M. M., Bland, R. C., Canino, G. J.,
Faravelli, C., Greenwald, S., Hwu, H. G.,
… & Yeh, E. K. (1994). The cross
national epidemiology of obsessive
compulsive disorder. The Journal of
Clinical Psychiatry, 55(Suppl), 5–10.
World Health Organization. (1992). The ICD
10 classification of mental and
behavioural disorders: Clinical
descriptions and diagnostic guidelines.