Introduction: Dissociative fugue is a rare mental health condition reported with a significantly
lower prevalence rate and presenting symptoms of amnesia along with the sudden onset of
travelling without knowing about self and whereabouts. There will be psychological trauma and
stressors in this health condition. The multidisciplinary team is effective in managing ongoing
psychosocial stressors impacting the episode. The current case study focuses on the psychosocial
aspect of the client who presented with such an illness. Assessment and diagnosis: This case
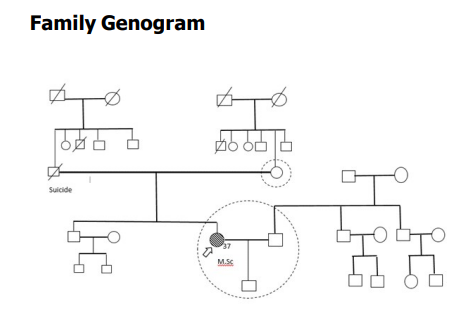
focusing on a 37 year old female diagnosed with recurrent depressive disorder and dissociative
fugue who had several psychosocial stressors in her family of origin and procreation. The client
was treated with pharmacological and non-pharmacological interventions. The Therapist has
done a psychosocial and family assessment and found poor functionality, assertiveness, and
interpersonal skills at the individual level. At the family level, interpersonal relationship issues
between client and spouse, poor communication, and poor understanding of the client’s condition
among spouse and caregiver burden were identified. Interventions: The psychosocial
intervention focuses on individual and family-level issues based on the assessment.
Psychoeducation, activity Scheduling, supportive psychotherapy, and couple therapy are the
primary interventions done during inpatient care. Conclusion: Psychosocial interventions are
more significant in dealing with even complicated illnesses. Intervention in communication and
interpersonal relationships will always give a better outcome. The multidisciplinary team approach
is essential in dealing with mental health issues.
Depression is considered as a common mental
health condition and 350 million people in the
globe suffer from depression, according to
the World Health Organization, and it accounts
for a higher burden according to years lost to
disability(YLD) (Smith, 2014). Depression is
a mood disorder with the symptoms of low
mood, loss of interest in all activity, decrease or increase in appetite almost all day, fatigue
or loss of energy, and feeling of worthlessness
that lasts for more than two weeks (American
Psychiatric Association, 2013). Recurrent
depressive disorder is a condition where at
least two depressive episodes should occur
with several-month gaps without any mood
disturbances (WHO, 2019). Major depressive
disorder is a mental illness that may have high
comorbidities (Hardeveld et al., 2009).
Dissociative fugue, formerly called
psychogenic fugue, is a group of psychiatric
conditions called dissociative disorders.
Dissociative fugue is the disruption of the
integration of consciousness, memory,
perception, identity, or emotion of the person
(Igwe, 2013). Dissociative disorders include
dissociative amnesia, fugue,
depersonalization disorder, dissociative
identity disorder, and dissociative disorder not
otherwise specified. (American Psychiatric
Association, 2000) Dissociative amnesia with
dissociative fugue is the “purposeful travel or
bewildered wandering associated with
amnesia for identity or other crucial
autobiographical information. (American
Psychiatric Association, 2013)
This case report is of a married woman with
recurrent depressive episodes and dissociative
fugue who had undergone traumatic life events
and psychosocial difficulties at the individual,
family, and social levels. The treating team
referred the patient to the psychiatric social
worker for psychosocial intervention at the
individual and family levels. The case report
highlighted the importance of psychosocial
intervention in recurrent depressive disorder
with a dissociative fugue. This case report can
elicit the scope of Psychiatric Social Workers,
their significance in a clinical setting, and
possible outcomes in a case study conducted
in NIMHANS, Bengaluru, Karnataka.
Case Introduction
A 37-year-old female educated up to M.Phil
in Microbiology was working as a hostel
warden hailing from middle socioeconomic
status, from Tamil Nadu
Source of Information,
Information was collected from the client, the
client’s husband, and the client’s son, as well
as from the case file in the medical record
department. The information was reliable and
adequate.
The client maintained well till 2014. However
when her husband compared her to his
colleague, who was also a family friend client
began to suspect him of having an extramarital
affair with that colleague. It became severe
when her husband went for exam preparation
for ten days and stayed in a hotel. The client
firmly believes that he spent those days with
the same colleague and enquired about them
in the hotel where he stayed. The hotel staff
refused to reveal her husband’s details,
making her more suspicious. She further
reported that the villagers spoke ill of her and
mocked her, which caused significant
emotional distress. During the same period,
she had a friendship with Mr P, who resides
in the same place. She collected his number
and contacted him by phone for three months.
In 2017, she had an episode of low mood, low
energy, decreased sleep, and reduced
interaction. She had several minor episodes
of fugue along with loss of memory.
Family History: Alleged history of suicide in
a first-degree relative. The client’s father died
by suicide when the client was 13 years old
and the reason was unknown.
Husband: is a 39-year-old male working as
a Lawyer. He was educated up to graduation
in law and did not report any health issues.
He was very bothered about his status and
had a social stigma regarding illness.
Criticality was present towards the client. He
was stressed and had burnout as he had to
manage many roles and responsibilities in the
house and workplace. He was ready for the
treatment and quite supportive. However, he
had poor knowledge about illness, which made
him more stressed. They have a good
relationship with each other after marriage.
Later, some issues arose in their relationship.
He was concerned about the treatment
period, the effectiveness of the medication,
and family life.
Wife: The index client. The client lives with
her husband and son. She was more attached
to her son. A cordial relationship was
maintained initially, and a communication
decline also existed in the latter part of their
lives.
Son: They had only one child, a 13-year-old
studying in the eighth standard. He was a easy
child who was very much attached to his
parents. He used to take care of his mother during her illness and was very much
concerned about his mother’s health. He is
emotionally supportive of his mother.
Boundary: The boundary of the family of
procreation was clearly defined and open.
Inference: The boundary was clear and open.
Subsystem: In this Family, two types of
subsystems exist. One was the couple
subsystem, and the other was the parent-child
subsystem. Both subsystems functioned well
earlier. A decrease in the functioning of a
couple subsystems existed during the past
four years. The illness affected the parentchild subsystem and significantly affected the
mother’s involvement.
Family developmental stage: The family is
in the IV stage of development, a family with
school-going children (Duvall, 2002). The son
is 13 years old and studying in the eighth
standard.
Leadership: The client’s husband is the
nominal leader in the family. The client less
involved in decision-making other than the
household chores. She reported less confident
in making decisions and expressing her
opinions. He ignored her as she responded
less and did not give suggestions. Hence, the
husband himself decides. The patient’s only
concern is that any decision regarding their
son should be discussed with her. Inference:
Leadership was accepted, and Democratic
decision-making was present
Role structure and functioning: Roles and
responsibilities are clearly defined in the
family. The client does household chores. Both
husband and client are earning. The client
takes care of the child and used to go to work.
Mutual support was present in the family. No
role confusion or conflict was reported. Due
to illness, there was decline in client
functioning and the husband took many of the
client’s roles before hospitalization. Inference: Complimentary, instrumental, and expressive
roles were present. The multiplicity of roles
is present in the husband.
Communication: Both verbal and nonverbal
communication was present in the family.
Communication among spouses was primarily
affected due to interpersonal relationship
issues among couples. Verbal communication
was also reduced between the client and the
son. The family had less expression of feelings
and emotions due to the illness. Inference:
Communication in the family of procreation
was affected due to the illness.
Reinforcement: The family has a positive
reinforcement mechanism. The husband and
son are attached to the client. The emotional
expression on the part of the client was less.
Positive and negative reinforcement was used
to rear the child. Inference: Both
reinforcements were present.
Family rituals: Initially, the family used to
have a standard time for sharing and
relaxation. Sometimes they go for an outing
and shopping or a picnic. During the past four
years, the quality of time spent by the
members was reduced. The family attended
religious functions and social gatherings.
Inference: Family rituals present.
Adaptive Pattern: The family uses good
adaptation and coping strategies to deal with
the problem. Over the past four years, the
communication gap affected the family’s
coping strategies. Inference: Positive coping
mechanisms and adaptive patterns were
present.
Social Support System: Primary Support:
Primary social support was present from
husband and son. Secondary Support:
Extended family members emotionally
supported the client and family. Tertiary
Support: NIMHANS, Bangalore is the tertiary
support for the family
Birth and early development: No reliable
informants were available.
Behavior during childhood: The client was
shy and inclusive during childhood. She had
fewer friends and less attachment to others.
Physical illness: No physical disease was
reported in childhood.
School: The client started schooling at the
age of six. She was an above-average student
and studied MPhil in Microbiology.
Occupation: The client worked as a hostel
warden for the past four years and travels
one and a half hour from her home. She had
three shifts in this job, significantly affecting
her sleep and changing her routine. Previously
she used to work as a liaison officer in the
information center of the Distance Education
department at Vadalur, which was 15 minutes
away from their home. It is a permanent job.
Menstrual history: The client attained
menarche at the age of 14 years. She had
regular periods and menstruation became
irregular in the past 12 months due to PCOD.
Sexual history: The onset of puberty was
at 13, and she learned about sex from friends
and books. She has had no extramarital
relationships. In 2016, spouses had no sexual
relationship for six months.
Marital history: The client married at the
age of 21 years, and the husband was 25
years old. It was a marriage by choice without
the consent of the family of origin.
A 37-year-old married female studied up to
post-graduation belongs to the middle
socioeconomic status from a Hindu religion,
born out of a non-consanguineous marriage
and history of suicide in father. She was
diagnosed with Recurrent Depressive
Disorder, Dissociative Fugue.
The psychosocial assessment revealed that
the client’s illness affected her social
functioning and her family. The client had poor
self-esteem and is an introvert by nature. She
had poor self-care, stress, problems in interpersonal relations and activities of daily
living, and deliberate self-harm behavior. At
the family level, there was interpersonal
relationship issues with her spouse, caregiver
burden, and poor communication in the family
of procreation. The assessment revealed that
she had single-parenting, and extended family
members were involved in the child’s rearing.
The client reported marital conflict among
parents, and the father’s death was a
traumatic stressful life-event in childhood. The
client’s family of origin had a close and rigid
boundary, and the mother carries out
instrumental roles. Decision-making was
democratic and later became authoritative.
Mother had complementary and multiple roles.
Communication was direct, and both types of
reinforcement were present. Family dynamics
in the family of procreation revealed that
communication and interaction between the
husband and the client were significantly
affected. The client used to do the routine
work very slowly and showed less interest in
talking with family members and spending
time with her son. The family interaction had
a moderate level of disruptions.
Psychoeducation is ‘systematic, structured,
didactic information on the illness and its
treatment, and includes integrating emotional
aspects to enable clients and family members
– to cope with the illness’ (Bauml, 2006). The
focus of psychoeducation may be compliance/
adherence-focused, illness-focused,
treatment-focused, and rehabilitationfocused. As per the Assessment, it was found
that the client lacked adequate knowledge
about her illness. The client was given a
medical model of explanation about her
condition of recurrent depressive disorder
with dissociation fugue. The Therapist
addressed the issue of self-harm during the
episodes. A detailed description of the nature
of the illness, symptoms, and causes, as well
as its effects on socio-occupational function,
treatment, and management, was given
during the session.
Activity scheduling (AS) is an effective
behavioral treatment that addresses social
isolation in clients with depression. It is an
approach that actively involves clients by
increasing the daily activities they do and
participate in (Lewinsohn & Atwood, 1969).
As her diagnosis was RDD with Dissociation
Fugue, engaging her in different activities is
essential, making her more productive and reducing her anxiety and other negative
thoughts. The client’s activities were carried
out according to the client’s wish, and the
client started following the activity, which was
scheduled gradually. The client started doing
the activities and functions in which she was
interested. The Therapist monitored the
activities and changed them according to the
client’s convenience. The client engaged in
maximum activities and utilized the yoga
center, library, and garden space effectively
Supportive psychotherapy is a form of
treatment whose principal concern and focus
is to strengthen mental functions that are
acutely or chronically inadequate to cope with
the demands of the external world and the
client’s inner psychological world. It enhances
the client’s strength, coping skills, and
capacity to use environmental supports and
reduces the client’s subjective distress and
behavioral dysfunction (Werman, 2014). Due
to family issues, clients have poor selfesteem, coping skills, assertive skills, and
distress. Individual sessions were conducted
to improve her self-confidence and selfesteem, and she also provided sessions on
problem-solving skills, decision-making, and
other life skills. Illness-related family issues
were also addressed, and relaxation
techniques for reducing distress were
provided. The Clinical Psychology team gave
assertive skill training, Grounding, emotion
regulation, and role-play.
Supportive psychotherapy was conducted after
formulating the case. It used strategies such
as therapeutic alliance, maximizing adaptive
coping mechanisms, and raising self-esteem
with various techniques such as guidance,
empathy, and verbal soothing, allowing the
client to ventilate and express her thoughts
and emotions (Misch, 2000). Family Casework
Family-centered casework is “ based on an
understanding of the social, physical and
emotional needs of the family as a unit for
the purpose of helping the family members
attain the best personal and social satisfaction
of which they are capable”. (Scherz, 1953)
Psychoeducation is a process by which mental
health professionals impart knowledge of the
illness to the family and, with continual
assistance, modify their attitude. It also
involves formulating and implementing better
coping skills and other preferred interactions
with the affected member (Varghese et al.,
2002). As per the Assessment, the family
consists of a husband and only son. The
Therapist explained to family members the
nature of the illness, its causes, and the role
of family support in improving the client’s
condition. They were educated about the
influence of stress and interpersonal
relationship issues on this illness. The
Therapist explained the symptoms, the
importance of treatment and medicine
adherence, and medication supervision.
The couple therapy sessions were based on
emotion-focused couple therapy, techniques
from the Gottman Method (Mordechai &
Schwartz, 2008), and other effective
communication techniques. The assessment
found that these couples have deficits in
severe areas, such as problems with
communication, intimacy, sharing, problemsolving, and decision-making. There is a lack
of attachment and bonding, and the therapist
used emotionally focused couple therapy to
deal with those issues. The Therapist
concentrated on their interactive pattern in
the home and how negatively it affects them.
The importance of being empathetic and
understanding each other was emphasized in the session. Couples have difficulty sharing
their emotions. The importance of sharing and
acceptance was explained. A considerable
communication gap was observed between
the couples, and the importance of effective,
open, and direct communication was also
specified in the session, along with
communication techniques. As pointed out in
consecutive sessions, appreciation and
gratitude are essential for good interpersonal
relationships. The Therapist used techniques
such as loving each other by understanding
the stress, emotion, and expectation,
appreciating each other, conversing with
interest and respect, building trust and
commitment, the balance of power, and
problem-solving skills used in the therapy.
The case report explored the impact of
psychosocial intervention on an individual and
family in a rare condition like a dissociative
fugue. The case work with the couples helped
to understand each other and fill up the lacuna
in several aspects of family dynamics and
interpersonal relationships. The session also
addressed the caregiver burden through the
micro-skills of active listening, paraphrasing,
and summarizing, which helped the client’s
husband improve his mental health—along
with psychiatric social work intervention
pharmacotherapy, individual therapy by
clinical psychologists and inpatient care also
played a significant role in improving client’s
psychiatric condition. The casework approach,
along with pharmacological treatment, shows
effective outcomes among persons diagnosed
with depression, which also substantiates this
study. (Keyho et al., 2020) The
biopsychosocial approach also shows a better
impact among people diagnosed with
depression, and the case report from Assam
states that a tailored psychiatric social work
intervention indicated a reduction in
symptoms as well (Bora et al., 2021).
Psychological intervention for dissociative
disorder found that supportive psychotherapy,
interpersonal skill development,
psychoeducation, and emotional regulation
skills can be a part of treatment along with
other psychological interventions.
(Subramanyam et al., 2020)
The case report shows the effectiveness of
psychosocial intervention among couples and
caregivers. The approach of the client’s
husband changed drastically at the end of the
intervention, and he accepted the patient with
the illness.
American Psychiatric Association. (2000).
Diagnostic and Statistical Manual of
Mental Disorders (DSM-IV-TR) (Text
Revision). American Psychiatric
Publishing.
American Psychiatric Association. (2013).
Diagnostic and Statistical Manual of
Mental Disorders V (Fifth Edition).
American Psychiatric Association.
Bauml, J. (2006). Psychoeducation: A Basic
Psychotherapeutic Intervention for Patients With Schizophrenia and Their
Families. Schizophrenia Bulletin,
32(Supplement 1), S1–S9.
Bora, D., Deuri, S. P., & Saha, A. (2021).
Psychiatric Social Work Intervention
with a Woman with Depression: A
Case Report from Assam.
International Journal of Indian
Psychology, 9(2), 1015-1022.
Duvall, E. M. (2002). Evelyn Duvall’s Life.
Marriage & Family Review, 32(1–2),
7–23.
Hardeveld, F., Spijker, J., De Graaf, R., Nolen,
W. A., & Beekman, A. T. F. (2009).
Prevalence and predictors of
recurrence of major depressive
disorder in the adult population:
Recurrence of major depressive
disorder. Acta Psychiatrica
Scandinavica, 122(3), 184–191.
Igwe, M. N. (2013). Dissociative fugue
symptoms in a 28-year-old male
Nigerian medical student: A case
report. Journal of Medical Case
Reports, 7(1), 143.
Keyho, K., Gujar, N. M., Ali, A., & Sahu, K. K.
(2020). Psychiatric social work
intervention with a person with severe
depression based on cognitive
behavioral casework approach: A case
study. Indian Journal of Psychiatric
Social Work, 11(1), 36.
Lewinsohn, P. M., & Atwood, G. E. (1969).
Depression: A clinical-research
approach. Psychotherapy: Theory,
Research & Practice, 6(3), 166–171.
Misch, D. A. (2000). Basic strategies of
dynamic supportive therapy. The
Journal of Psychotherapy Practice and
Research, 9(4), 173–189.
Mordechai, G. J., & Schwartz, G. J. (2008).
Gottman method couple therapy.
Clinical Handbook of Couple Therapy,
A. S. Gurman (Ed.) (The Guilford
Press), 138–164.
Scherz, F. H. (1953). What is Family-Centered
Casework? Social Casework, 34(8),
343–349.
Smith, K. (2014). Mental health: A world of
depression. Nature, 515(7526), 180–
181.
Subramanyam, A., Somaiya, M., Shankar, S.,
Nasirabadi, M., Shah, H., Paul, I., &
Ghildiyal, R. (2020). Psychological
Interventions for Dissociative
Disorders. Indian Journal of
Psychiatry, 62(8), 280.
Varghese, M., Shah, A., Kumar, G. U., Murali,
T., & Paul, I. M. (2002). Family
interventions and support in
schizophrenia: A manual on family
intervention for the mental health
professionals. WHO/National Institute
of Mental Health and Neuro Science.
Werman, D. S. (1989). Practice of Supportive
Psychotherapy ( 1st ed.). Routledge.
WHO, W. H. O. (2019). International Statistical
Classification of Diseases and Related
Health Problems (ICD-11) (11th Ed).