This case study explores the complex interplay between parental pressure, academic stress, and
depression The study aims to assess psycho-social factors and evaluate the effectiveness of
psycho-social interventions in managing depression. This single-subject case study assesses the
effectiveness of the bio-psycho-social model in understanding depression and its treatment through
psychiatric social work intervention. Employing pre- and post-intervention baseline assessments,
the study utilizes various tools including the Family Assessment Device (FAD), Beck Depression
Inventory (BDI), Beck Anxiety Scale, Self-Esteem Scale, Multi-Dimensional Perceived Social Support
Scale, Perceived Stress Scale, a family questionnaire, Internet Addiction Scale, Brief Sex Addiction
Screening Instrument (PATHOS), and the Five Facet Mindfulness Questionnaire (FFMQ). The
case was referred for assessment and intervention. The intervention comprised CognitiveBehavioural Therapy (CBT)and mindfulness-based intervention. Additionally, the family intervention
was provided to address parental academic pressure towards the patient and educate the family
members about the illness. Following Psychosocial intervention, there were significant changes
in pre- and post-intervention scores across various domains, stress, depression, anxiety, selfesteem, internet addiction, pornography addiction, and mindfulness. The study underscores the
effectiveness of psycho-social interventions in addressing depression influenced by academic
and parental pressures.
Adolescence is a critical developmental stage
characterized by extensive changes and
heightened vulnerability to psychological
disorders such as anxiety and
depression(Sawyer, Azzopardi,
Wickremarathne, Patton, 2018 & McCanceKatz, 2018). This vulnerability is exacerbated
by academic pressures and high-stress family
environments, which contribute significantly
to the risk of mental health issues, including
suicidal ideation. Parenting styles marked by
inconsistency, harsh discipline, and emotional
detachment further complicate adolescents’
emotional and social development, negatively
affecting their academic performance and
social relationships. Despite the availability of
treatments like cognitive-behavioural therapy
(CBT) (Hofmannet, 2012). and mindfulness based cognitive therapy (MBCT) (Goldberg et
al.,2018 & Strauss et al.,2014) which have
been proven effective in managing symptoms
of depression and anxiety, there is a notable
deficiency in interventions specifically tailored
to address the unique challenges faced by
adolescents dealing with academic and
familial stress The intervention intends to
reduce stress and enhance overall
psychological well-being by addressing the
specific psychosocial factors that impact this
age group. This approach is crucial for
developing more targeted and effective mental
health support for adolescents, thereby
improving their long-term outcomes in both
academic and personal spheres. Family
interventions can play a crucial role in treating
adolescent depression by addressing
interpersonal dynamics that may contribute
to the condition(Diamond & Josephson, 2005).
Effective family psychoeducation, focusing on
understanding depression through a medical
model, educating on patient-specific issues,
and teaching about stress vulnerability and
coping strategies, has shown promising
results. Such interventions not only reduce
depressive symptoms in the short term but
also enhance social functioning and improve
relationships with parents and peers,
contributing to long-term mental health
benefits for adolescents. The effectiveness of
existing interventions varies, and there
remains a significant gap in targeted
psychosocial strategies that address the
specific needs of adolescents experiencing
academic and familial stress. This
underscores the importance of a tailored
approach that considers the psychosocial
factors influencing adolescent mental health.
Therefore, this study seeks to evaluate the
impact of a comprehensive psychosocial
intervention designed to alleviate stress and
improve the psychological well-being of the
client.
This study employs a single case study design
to assess the effectiveness of a psychosocial
intervention based on the biopsychosocial
approach for individuals with moderate
symptoms of depression and anxiety. Pre and
post-intervention baseline data are compared
to evaluate changes in the client’s condition.
The present case was purposefully selected
from the Outpatient Department of tertiary
care institute in Delhi. Before the
commencement of the study, informed
consent was obtained from the client’s father,
mother, sister, and teachers, as well as from
the client himself. Participants were assured
about the confidentiality of their information
and were provided with detailed information
about the nature and purpose of the study.
Baseline data were collected before the
commencement of the psycho-social
intervention. Using a standardised scale.
Family Assessment (FAD)(Epstein,Baldwin, &
Bishop, 1983)Beck Depression Inventory (BDI)
(Beck et al.,1961), Beck Anxiety Scale(Beck,
Steer, 1990), Self-Esteem Scale(Rosenberg ,
1965). Multi-Dimensional Perceived Social
Support Scale(Zimet,Dahlem, Zimet & Farle,
1988). Perceived Stress Scale(Cohen,
Kamarck & Mermelstein, 1983). Internet
Addiction Scale(Young, 1998).Brief sex
addiction screening instrument (PATHOS)
(Carnes et al.,2012)and the Five Facet
Mindfulness Questionnaire (FFMQ) (Baer,
2006) were administered. Ethical guidelines
and principles were followed throughout the
study to ensure the rights, dignity, and
confidentiality of the participants.
Mr. X an 18-year-old single male, currently
pursuing his Bachelor’s degree from IGNOU
while simultaneously preparing for civil
services exams, was brought to Tertiary care
centre by his father. He presented with chief
complaints of anxiousness, low mood, lack of interest in work, chest pain, restlessness,
overthinking, stomach pain, and
preoccupation with health concerns.Mr. X hails
from a middle socio-economic status rural
background, with both parents engaged in
farming and cattle rearing. His parents held
high expectations for him to succeed in the
civil services exams, leading to his enrollment
in coaching classes in Delhi. Despite facing
difficulties in keeping up with his studies and
enduring a daily five-hour commute to and
from the coaching centre, Mr X did not
communicate his struggles to his parents and
continued attending classes regularly.
Described as introverted, Mr.X refrained from
expressing his problems to his family and
preferred solitude in his room. During study
breaks, he began watching pornography
videos on his mobile phone, eventually
developing an addiction. This behavior change
was noted by his family, along with complaints
of headaches, stomach pains, and chest pains.
Concerned about his well-being, Mr. X’s father
sought professional help. Upon assessment,
Mr. X was diagnosed with moderate
depression, and treatment was initiated
alongside a referral for psychosocial
intervention. In response to his condition, a
comprehensive treatment plan was developed,
which included both pharmacological and
psychosocial interventions. Therapy sessions
were initially scheduled on a monthly basis
for one year to establish a foundation for
treatment and address his immediate needs.
Following this period, sessions were planned
bi-monthly to continue addressing his mental
health concerns and support his ongoing
recovery. The therapeutic approach help the
client to manage his depression, cope with
stress more effectively, and address his
pornography addiction while gradually
improving his overall well-being and quality
of life.
Mr. X exhibits symptoms of depression and
anxiety, including low mood, somatic
complaints, poor sleep, and decreased
appetite. These symptoms suggest
dysregulation of neurotransmitters and the
autonomic nervous system, potentially
contributing to his mental health struggles.
Mr.X’s introverted personality, poor coping and
problem-solving skills, and low self-esteem
further exacerbate his mental health
challenges. These psychological factors may
hinder his ability to effectively communicate
and manage stressors, leading to maladaptive
behaviours such as excessive mobile use and
addiction. Family dynamics play a significant
role in Mr. X’s mental health. The pressure
from his parents to excel academically,
combined with a dominant father and
submissive mother, contributes to
communication difficulties and feelings of
inadequacy.Additionally, maladaptive parentchild communication and a high degree of
aversiveness in the family environment further
impact Mr. X’s emotional well-being. Mr. X’s
mental health struggles arise from a complex
interplay of biological, psychological, and
social factors. Biological factors such as
neurotransmitter dysregulation contribute to
his symptoms of depression and anxiety.
Psychological factors, including introversion,
poor coping skills, and low self-esteem,
exacerbate his distress and hinder his ability
to manage stressors effectively. Social
factors, particularly parental pressure and
communication difficulties within the family,
create a stressful environment that
perpetuates Mr X’s mental health challenges.
A total of 24 individual and 4 family therapy
sessions were conducted as part of the
intervention. Rapport was established with the
client and their family, and informed consent
was obtained before the commencement of therapy. Clear goals were set collaboratively
between the therapist and the client, and
detailed information about the therapeutic
process, including the timing and duration of
sessions, was provided. This ensured that the
client and their family were fully informed and
engaged in the therapy process, promoting a
supportive and collaborative therapeutic
relationship.In the cognitive-behavioural
therapy (CBT) sessions conducted for Mr. X
the ABC model was employed to address his
depression. The ABC model framework was
used in CBT to help the client understand the
connection between their thoughts, emotions,
and behaviours. During the CBT sessions, the
focus was on modifying underlying schemas
or core beliefs that were contributing to Mr.
X’s depression. By identifying and challenging
maladaptive schemas related to self-worth,
achievement, and coping, Mr. X learned to
adopt more adaptive ways of thinking.
Throughout the CBT sessions, a rapport was
established between Mr. X and the therapist,
creating a safe and supportive environment
for exploration and change. Clear goals were
set collaboratively between Mr. X and the
therapist, providing direction and motivation
for the therapeutic process. Regular
assessments were conducted to track Mr. X’s
progress and adjust the treatment plan as
needed. Overall, CBT proved to be an effective
intervention for Mr. X offering practical
strategies for reducing depressive symptoms,
modifying underlying beliefs, and improving
coping skills. By addressing the cognitive and
behavioural aspects of his depression, Mr X
was able to manage his mental health and
enhance his overall well-being.
We addressed internet addiction and
pornography use through cognitive
restructuring techniques within Cognitive
Behavioral Therapy (CBT). The client was
introduced to cognitive restructuring, which
helps in recognizing and modifying distorted
thought patterns that influence behavior. We
discussed how the client might use online
activities as a substitute for real-life selfesteem boosts and encouraged them to
identify when they use the internet as an
escape or to satisfy unmet needs rather than
addressing these needs directly. The session
focused on evaluating the rationality and
validity of the client’s current beliefs about
internet use and pornography. We also
worked on recognizing patterns of faulty
thinking, which will aid the client in challenging
these thoughts outside of therapy. The
discussion highlighted the difficulties in
justifying excessive internet use once the
client becomes aware of these thought
patterns and emphasized finding healthier
ways to meet unmet needs and build selfesteem without relying on the internet.
Techniques for stress management and urge
reduction, such as deep breathing and
progressive muscle relaxation, were
introduced. Additionally, mindfulness
strategies were taught to increase awareness
of emotional and behavioral patterns. By
integrating these mindfulness practices into
their daily routine, the client was encouraged
to build resilience against depressive and
anxious thoughts, ultimately enhancing their
emotional well-being. We developed a plan
for better time management to decrease
online time and boost real-life engagement.
The client demonstrated a willingness to
engage in cognitive restructuring and is
beginning to understand the link between
their thought patterns and internet use..
Family Interventions were provided focusing
on building parenting skills and promoting
positive parenting practices that can help to
reduce stress. Education was provided about
child development, his mental health status,
and realistic expectations of parenting that can
help reduce stress by aligning parental
expectations with reality.
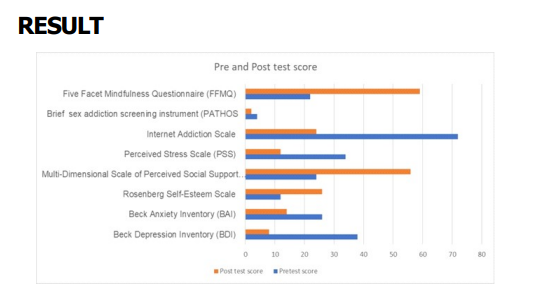
Figure 1 illustrates changes in pre- and postscore in the Beck Depression Inventory (BDI),
Beck Anxiety Inventory (BAI), Rosenberg SelfEsteem Scale, Multi-Dimensional Scale of
Perceived Social Support (MSPSS), Perceived
Stress Scale (PSS) , Internet Addiction Scale,
Brief sex addiction screening instrument
(PATHOS and Five Facet Mindfulness
Questionnaire (FFMQ).
Psychosocial interventions were provided to
the patient, the session was mainly based on
cognitive-behavioural therapy (CBT), which
significantly improved the overall well-being
of the client. These interventions led to a
noticeable reduction in symptoms of
depression, anxiety, and stress. The psychosocial intervention specifically addressed
behavioural addictions such as internet
gaming and pornography in the client by
utilising CBT and mindfulness techniques, the
client saw notable improvements in postsession. Mindfulness-based strategies were
also implemented to help manage stress more
effectively. These comprehensive approaches
not only targeted the reduction of problematic
behaviours but also enhanced the client’s
ability to cope with daily stressors,
contributing to their mental health recovery
and improved quality of life. Cognitivebehavioral therapy (CBT) offers a potent
remedy for managing such stresses by helping
individuals identify and modify harmful
thought patterns that adversely affect their
behavior and emotions. Mindfulness-based
cognitive therapy (MBCT) also significantly
reduces depression symptoms in current
sufferers and is as effective as other
established treatments like group CBT
(Hofmann et al.,2012 and Strauss et al., 2014)
. Family interventions, too, play a crucial role.
After such interventions, there is often marked
improvement in mental health, with significant
reductions in depression, anxiety, and stress
observed. These interventions also help
families understand the illness better and
provide more supportive environments for the
patient. Support systems, particularly through
parental involvement and fostering positive
home environments, are vital for mitigating
academic stress. Adolescents with strong
parental support and minimal negative
interactions are better equipped with coping
skills (Klootwijk et al.,2021). illustrating the
importance of a nurturing home in combating
the adverse effects of academic pressures.
The findings highlight the efficacy of
psychosocial interventions, particularly
Cognitive Behavioral Therapy (CBT), in
managing depression and behavioral
addictions, such as internet gaming and
pornography, in the client. These
interventions play a crucial role in alleviating
the impact of academic pressure and
addressing the underlying mental health
issues. Psychosocial approaches, including
CBT, Mindfulness-Based Cognitive Therapy
(MBCT), and family therapy, are essential in
navigating the complex interplay of academic
stress, family dynamics, and mental health
challenges. By integrating these therapeutic
modalities, the treatment effectively mitigates
the negative effects of academic and familial
pressures, supports the client in overcoming
behavioral addictions, and fosters overall
emotional well-being. The comprehensive
nature of these interventions underscores
their importance in addressing multifaceted
issues and promoting sustainable recovery.
Baer R. A., Smith, G. T., Hopkins, J.,
Krietemeyer, J., & Toney, L. (2006).
Using self-report assessment methods
to explore facets of mindfulness.
Assessment, 13(1), 27-45.
Beck, A. T., & Steer, R. A. (1990). Beck Anxiety
Inventory Manual. San Antonio, TX:
Psychological Corporation
Beck, A. T., Ward, C. H., Mendelson, M., Mock,
J., & Erbaugh, J. (1961). An inventor
for measuring depression. Archives of
General Psychiatry, 4(6), 561-571.
Carnes PJ, Green BA, Merlo LJ, Polles A,
Carnes S, Gold MS. PATHOS(2012) A
brief screening application for
assessing sexual addiction. J Addict
Med.6(1):29–34.
Cohen, S., Kamarck, T., & Mermelstein, R.
(1983). A global measure of perceived
stress. Journal of Health and Social
Behavior, 24(4), 385-396.
Diamond G , Josephson A (2005) Family-based
treatment research: a 10-year
update . J Am Acad Child Adolesc
Psychiatry . 44 : 872 – 887
[PubMed] [Google Scholar] [Ref list]
Epstein, N. B., Baldwin, L. M., & Bishop, D. S.
(1983). The McMaster Family
Assessment Device. Journal of Marital
and Family Therapy, 9(2), 171-180.
Goldberg SB, Tucker RP, Greene PA, Davidson
RJ, Wampold BE, Kearney DJ, Simpson
TL(2018). Mindfulness-based
interventions for psychiatric disorders:
A systematic review and metaa n a l y s i s . C l i n i c a l
PsychologyReview59:52–60. [PMC
free article ] [PubMed] [Google
Scholar
Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT,
Fang A(2012). The efficacy of
cognitive behavioral therapy: a review
of meta-analyses. Cognit Ther
Res.36:427–440.
Klootwijk CLT, Koele IJ, van Hoorn J, Güroðlu
B, van Duijvenvoorde ACK.(2021)
Parental Support and Positive Mood
Buffer Adolescents’ Academic
Motivation During the COVID-19
Pandemic. J Res Adolesc.
Sep;31(3):780-795. doi: 10.1111/
jora.12660. PMID: 34448292; PMCID:
PMC8456955
McCance-Katz E. (2018) The substance abuse
and mental health services
administration (SAMHSA): new
directions. Psychiatr Serv. 69:1046–
8. 10.1176/appi.ps.201800281
[PubMed] [CrossRef] [Google Scholar
Rosenberg, M. (1965). Society and the
adolescent self-image. Princeton, NJ:
Princeton University Press.
Sawyer SM, Azzopardi PS, Wickremarathne
D, Patton GC.(2018) The age of
adolescence. The Lancet Child &
Adolescent Health.;2(3):223–8.
https://doi.org/10.1016/S2352-
4642(18)30022-1
Strauss C, Cavanagh K, Oliver A, Pettman
D( 2014). Mindfulness-based
interventions for people diagnosed
with a current episode of an anxiety
or depressive disorder: A metaanalysis of randomised controlled
trials. PLoSOne. 9(4):e96110. [PMC
free article ] [PubMed] [Google
Scholar]
Young, K. S. (1998). Internet addiction: The
emergence of a new clinical disorder.
CyberPsychology & Behavior, 1(3),
237-244.
Zimet, G. D., Dahlem, N. W., Zimet, S. G., &
Farley, G. K. (1988). The
Multidimensional Scale of Perceived
Social Support. Journal of Personality
Assessment, 52(1), 30-41