Background: Conduct Disorder (CD) is a childhood disorder marked by consistent anger, defiance,
and a desire for revenge. Children with CD struggle to control their emotions and actions. It
affects about 5-8% of children globally and typically starts between the ages of 10 and 18 years.
Methods and Materials: The three index clients, male, between 12-14 years of age, visited
the Institute of Psychiatry, Kolkata, with caregivers and were referred to the Psychiatric Social
Work department with the symptoms of stealing, lying, blaming, cruelty towards animals, anger
outbursts, hitting behavior towards others, and poor treatment adherence. Gradually titrating
the doses upwards, Tablet Risperidone upto a dose of 04 mg/day was prescribed to all of them.
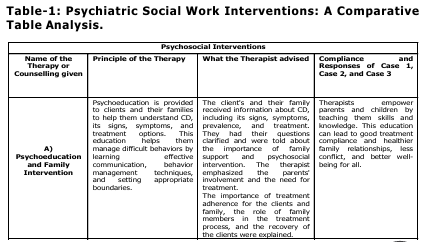
Following, the Psychiatric Social Worker imparted parent management training, behavior therapy,
parent-child interaction training, and anger management to the clients and family members.
Results: After the Psychiatric Social Work (PSW) interventions in combination with medication,
there were noticeable improvements in the lives and well-being of individuals with CD and their
families. The severity of CD symptoms decreased, high emotional expression decreased, and
family cohesion improved. Both clients and family members learned how to prevent recurrent
symptoms in future issues. Risperidone was tapered off in two individuals and in one, it was
reduced to 0.5 mg/day following the PSW interventions, once symptom control was achieved.
Conclusion: PSW interventions play a crucial role in managing Conduct Disorders (CD) by
involving the family. This approach helps in sustaining long-term well-being and improving
treatment (pharmacological and non-pharmacological) adherence.
Conduct disorder is a complex condition
marked by persistent behavioral and
emotional challenges in children. Those
children and adolescents find it hard to
adhere to rules, empathize with others, and
behave in socially acceptable ways, often leading to negative perceptions from peers,
adults, and social agencies. Diagnosing
Childhood Onset Conduct Disorder in young
children is challenging because they often
struggle to express their feelings. Symptoms
can vary depending on the child’s
developmental stage. For a diagnosis, at least
one symptom of conduct disorder must be
present before the age of 10(American
Psychiatric Association. (2013), these
symptoms may include aggression toward
people or animals (e.g., bullying, physical
fights, cruelty to animals), destruction of
property (e.g., deliberate fire-setting or
vandalism), deceitfulness or theft (e.g., lying
to obtain goods or favors, shoplifting), and
serious violations of rules (e.g., truancy from
school, running away from home). Identifying
these behaviors early is critical for timely
intervention and effective management.
Childhood Onset Conduct Disorder is
influenced by biological and psychosocial
factors and is more common in boys across
all groups. Associated social factors include
poverty, low socioeconomic status, parental
issues, poor education, weak community
support, academic struggles, and unstable
families (Loeber, R., & Keenan, K., 1994), also
included marital problems, inability to improve
their situation, poor discipline methods, lack
of interest in treatment, and mental health
challenges among family members (Sajadi et.
al.,2020). The prevalence of conduct disorders
affects 5-8% of all children, with a subset of
2-6% affected between ages 4 and 18. Among
youth under 18, CD rates are higher in boys
(6-16%) compared to girls (2-9%) (Gitonga
et.al., 2017). In India, it is found that the
prevalence of conduct disorders increased for
both males and females across all socio
economic groups, specifically, the increase
was noted at a rate of 4.58% for boys and
4.50% for girls (Agarwal & Sao,2014).
Various factors contribute to conduct
disorders, including genetics, academic
challenges, and the environment.
Understanding these factors is crucial for
supporting those affected by the disorder
(Scott, S, 2018). A chaotic home environment
with insufficient structure and supervision,
along with frequent parental conflicts, can lead
to problematic behavior in children. This may
result in harsh or punitive parenting,
negligence, exposure to domestic violence,
and an increased risk of neglect and emotional
instability for the child (American Psychiatric
Association. (2013). Early intervention is
crucial to prevent worsening antisocial
behavior in adulthood.
This study emphasizes the significance of
therapy for children with conduct disorder in
combination with medication. It investigates
whether PSW intervention can lessen problem
behavior, enhance family relationships, and
encourage treatment adherence. The aim is
to prevent recurrent symptoms in the future,
reduce caregiver stress, promote well-being
and treatment adherence, improve
communication patterns, and parent-child
relationships in the family.
Index client, 12 years old, Hindu, Bengali,
male, coming from semi urban area, low
socio-economic status, studied in class VI,
presenting with the complaints of demanding
behavior, hitting towards mother, use abusive
language for last 1 1D 2 years, Stealing,
laying, blaming for last 1.5 years, with
i nsidious onset, continuous course,
deteriorating progress, Poor treatment
compliance, Personal history revealed
behavioral problem like restlessness,
inattentive, limited number of friends, With
Family dynamics suggestive of diffuse
boundary, Parent child subsystem absent
between client and his father, non-verbal and
switch board communication present between client and his father, high noise levels.
Reinforcement is absent with inadequate
cohesiveness. Behavior observation revealed
i rritable affect, intact orientation, but
impaired memory function.
Index client, 12-year-old, Hindu, Bengali,
male, coming from semi urban area, low
socio-economic status, studied in class VI,
who has trouble following his parents’
instructions mostly, gets angry easily from 1.2
years demands a lot, harming his younger
brother from 1.8 years and shows aggressive
behavior towards animals and others and
excessively fond of mobile using from last 02
years with insidious onset, continuous course,
deteriorating progress, with poor treatment
compliance, Family dynamics appear to be
contributing to the client’s behavior, with a
diffuse boundary and poorly formed
subsystems between the parents and the
client and his brother. The father’s autocratic
l eadership style and the mother’s role
multiplicity. Interaction patterns within the
family are described as need-based and
strained, particularly with the younger
brother. High noise levels, emotional burden,
inadequate reinforcement, and cohesiveness
within the family environment are present.
There are personal history indicators such as
restlessness, inattention, limited friendships,
and difficulties with concentration and
memory.
Index client, 14-year-old, Hindu, Bengali, male
coming from rural area, low socio-economic
status, studied in class VII, has been showing
demanding behavior, hitting family members,
using abusive language for four years, and
setting fire at home, cruelty to animals,
stealing from home for the past two years,
with insidious onset, continuous course,
deteriorating progress with poor treatment
compliance, Personal history, he’s shown
temper tantrums towards classmates and has
only a few friends. Family dynamics indicate
a diffuse boundary, with his father as an
autocratic and nominal leader. Communication
with his father is non-verbal and a
switchboard. There’s a high noise level,
emotional burden present in the family, and
inadequate adaptive patterns. The mental
status examination displayed hand tremors.
He showed a delayed reaction time and
appeared irritable, with difficulties in attention
and concentration.
To help three adolescents with conduct
disorder, we start by understanding the causes
of their behavior through counseling and
checklists. Then, we provide tailored
interventions over 12 sessions, including
coping and social skill training individually and
family-level support like psychoeducation and
improving family interactions.
In the beginning, individual sessions focus on
building rapport. Then, over five sessions, the
approach becomes more directive. During the
assessment session, we observe both
behavioral excesses and deficits. Family
sessions
mainly
concentrate
on
psychoeducation and enhancing family
i nteraction patterns. This intervention
supports and addresses underlying issues.
Family intervention deals with family
dynamics, while individual counseling offers
personalized support. Overall, seven sessions
were needed for this intervention
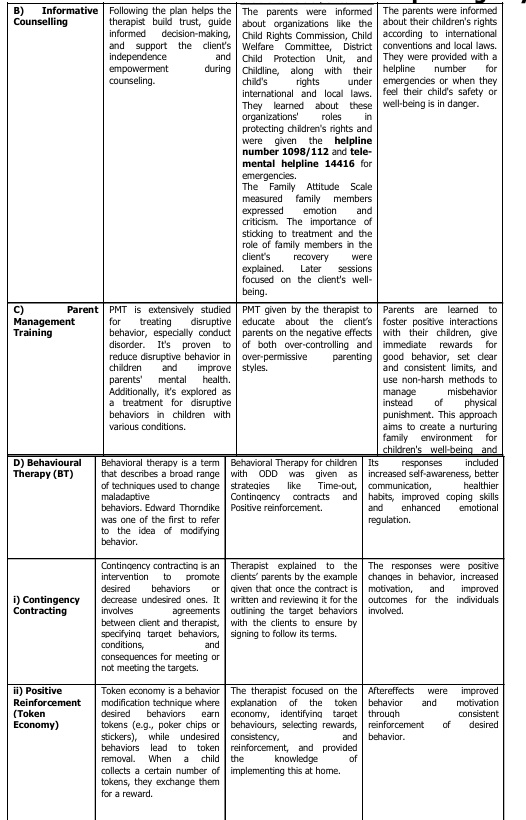
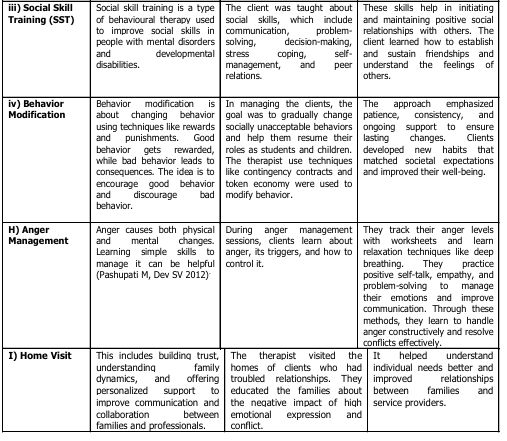
During regular follow-up sessions, clients and
their families participated, with feedback
recorded, and Child Symptoms Inventory and
Family Attitude Scale assessments were
conducted. By the 12th session, clients showed
remarkable improvement, attending school
consistently and reducing problem behaviors.
Both parents expressed satisfaction with their
progress and were reminded of the
importance of consistent parenting. It has
been noticed that due to PSW intervention in
case 01 Risperidone dose was gradually
reduced to 0.5 mg/day and in case 02 & 03,
Risperidone was tapered off and stopped.
Table 2: Pre- and Post-Intervention
Assessment to measure the level of
severity of Conduct Disorder.
This study highlights the significant
improvements in both child behavior and
family dynamics following psychosocial
interventions for children with Conduct
Disorder (CD). Pre- and post-intervention
revealed a marked reduction in CD symptoms
and high-expressed emotions like critical
comments and hostility, alongside increased
positive expressed emotions like family
warmth, support, and positive interactions.
Tailored treatment plans, combining
psychotherapy, medication, and family
focused strategies, addressed the challenges
of CD, with Parent Management Training (PMT) playing a pivotal role in reshaping family
dynamics. By empowering parents with non
harsh disciplinary techniques and reinforcing
positive behaviors, these interventions
fostered stability, emotional bonding, and
structured routines at home. Behavioral
therapies, including Contingency Contracting,
Token Economy, and Social Skills Training,
enhanced emotional regulation and social
competence; while anger management
sessions helped children manage triggers and
conflicts effectively. Positive changes in
parental attitudes were observed early,
demonstrating the rapid impact of these
interventions. This study underscores the
importance of a comprehensive, family
inclusive approach and emphasizes the need
for sustainable support systems to maintain
progress.
However, achieving full healing requires
ongoing commitment and support.
Researchers, like Helander et al. (2022),
agree with this study’s findings. They support
the effectiveness of combining Parent
Management Training (PMT) with Cognitive
Behavioral Therapy (CBT) for children with
Conduct Disorder (CD) and their families.
Similarly, A study by Loeber and Keenan
(1994) found that psychosocial interventions,
including Parent Management Training (PMT),
significantly improved children with Conduct
Disorder (CD) and their families. These
interventions helped address family dynamics,
stabilize routines, and encourage positive
behavior. Positive changes in parental behavior
were observed after just a few sessions,
showing the effectiveness of the approach. A
study also aligns with this, showing a link
between expressed emotion, caregivers’
stress, and the child’s self-sufficiency
(Balachandran et. al., 2023). No studies
contradict these results or the treatment
approach used in this study.
CONCLUSION
Our investigation has uncovered the profound
impact of psychiatric social work interventions
in combination with medication on children
struggling with Conduct Disorders (CD) and
t heir families. Through the strategic
application of therapeutic techniques such as
Parent Management Training (PMT),
Behavioral Therapy (BT), and Anger
Management, we witnessed significant strides
forward. The effects of these interventions
were not confined to the individual children
alone; rather, they resonated throughout the
familial ecosystem. Observable changes in the
children’s behavior included a palpable
reduction in disruptive tendencies and a
notable enhancement in academic
performance, underscoring the efficacy of our
therapeutic approaches. Furthermore, the
ripple effect extended to the dynamics within
the family unit. Decreased discord and
heightened cohesion emerged as hallmarks of
the familial transformation, contributing not
only to a more harmonious domestic
environment but also to the overall well-being
of each family member. Of particular
significance was the assimilation of preventive
measures by both children and their families.
Empowered with new strategies and coping
mechanisms, they found themselves better
equipped to confront the complexities of
future challenges with resilience and
determination, thereby laying a sturdy
foundation for sustained growth and progress.
Agarwal, M., Hemadri, K., & Sao. (2014).
Conduct disorder among adolescents:
An intervention approach through
psycho-yogic
program. The
International Journal of Indian
Psychology, 2(1), 269–271. https://
ijip.in/wp-content/uploads/2019/02/
10-M-Agarwal-H-Sao.pdf
American Academy of Child and Adolescent Psychiatry.
(1997). Practice
parameters for the assessment and
treatment of children and adolescents
with conduct disorder. Journal of the
American Academy of Child &
Adolescent Psychiatry, 36(10 Suppl),
122S–139S. https://doi.org/10.1097/
00004583-199710001-00008
American Psychiatric Association.
(2021). Diagnostic and statistical
manual of mental disorders (DSM-5).
American Psychiatric Publishing.
Balachandran, K. P., & Bhuvaneswari, M.
(2023). Expressed emotion in families
of children with neurodevelopmental
disorders: A mixed-method approach.
Annals of Neurosciences. https://
doi.org/10.1177/09727531231181014.
Gitonga, M., Muriungi, S., & Ongaro, K.
(2017). Prevalence of conduct
disorder among adolescents in
secondary schools: A case of
Kamukunji and Olympic mixed sub
County secondary schools in Nairobi
County, Kenya. African Journal of
Clinical Psychology, 1, 100. https://
www.daystar.ac.ke/ajcp/download/6/
1662453869_Prevalence-of-Conduct
Disorder-among-Adolescents-in
Secondary-Schools.pdf
Helander, M., Asperholm, M., Wetterborg, D.,
Öst, L., Hellner, C., Herlitz, A., &
Enebrink, P. (2022). The efficacy of
parent management training with or
without involving the child in the
treatment among children with clinical
levels of disruptive behavior: A meta
analysis. Child Psychiatry & Human
Development, 55(1), 164-181. https:/
/doi.org/10.1007/s10578-022-01367
y
Loeber, R., & Keenan, K. (1994). Interaction
between conduct disorder and its
comorbid conditions: Effects of age
and gender. Clinical Psychology
Review, 14(6), 497–523. https://
d o i . o r g / 1 0 . 1 0 1 6 / 0 2 7 2
7358(94)90015-9
Pashupati, M., & Dev, S. V. (2012). Anger and
its management. Journal of Nobel
Medical College, 1(1), 9–14.
Sajadi, S., Raheb, G., Maarefvand, M., &
Alhosseini, K. A. (2020). Family
problems associated with conduct
disorder perceived by patients,
families, and professionals. Journal of
Education and Health Promotion, 9,
184. https://doi.org/10.4103/
jehp.jehp_110_20
Scott S. Conduct disorders. In Rey JM (ed),
IACAPAP e-Textbook of Child and
Adolescent Mental Health. Geneva:
International Association for Child and
Adolescent Psychiatry and Allied
Professions, 2012.