Osteoarthritis (OA) is a prevalent musculoskeletal disorder with significant impact on patient
well-being and healthcare systems. This case study presents two patients in India with OA resulting
from traumatic injuries, comparing two reportorial methods in homeopathic remedy selection.
The first case (Male, 56) used the elimination method, emphasizing past injury, leading to the
selection of Sulphuricum Acidum, a constitutional remedy. In contrast, the second case (Male,
58) applied the totality method, which focused on the complete symptom picture, resulting in the
prescription of Bryonia. Both methods proved effective, demonstrating the importance of tailored
approaches in homeopathic practice. Treatment combined non-pharmacological strategies such
as exercise, weight management, and assistive devices, with pharmacological options like
acetaminophen and topical NSAIDs for pain relief. Despite initial improvements, corticosteroid
injections and physical therapy were required for ongoing symptoms. This case highlights the
complexity of OA management in India, emphasizing early detection, diverse treatment
approaches, and long-term patient care.
Osteoarthritis (OA) is a prevalent
degenerative joint disorder characterized by
cartilage degradation, subchondral bone
remodeling, and synovial inflammation. It
primarily affects weight-bearing joints,
causing pain, stiffness, joint effusion, and
functional impairment. Aging, genetic
predisposition, biomechanical stress,
metabolic dysregulation, and inflammatory
mediators contribute to OA development
(Felson & Zhang, 1998; Felson et al.,
2008).The pathogenesis of OA involves
abnormal chondrocyte metabolism,
imbalanced extracellular matrix turnover,
oxidative stress, and inflammation, with
cytokines such as IL-1â and TNF-á playing key
roles (Felson et al., 2000; Abramson & Attur,
2009). Recent research highlights the
influence of epigenetics, mitochondrial
dysfunction, and dysregulated autophagy in
OA progression (Bijlsma et al., 2011).
Management options are mainly palliative,
including lifestyle modifications, physical
therapy, analgesics, NSAIDs, corticosteroid
injections, and viscosupplementation
(Hochberg et al., 2012). However, challenges persist due to delayed diagnosis, limited
treatment efficacy, and the lack of diseasemodifying therapies. There is a pressing need
for innovative strategies to enhance OA
diagnosis and treatment (Hunter et al., 2014).
In India, factors like manual labor, squatting,
poor ergonomics, and rising obesity rates
exacerbate OA (Brown et al., 2006). Genetic
predispositions and pro-inflammatory dietary
patterns further contribute to its pathogenesis
(Gelber et al., 2008). Previous joint injuries,
malalignment, and metabolic syndrome also
increase OA risk (Brown et al., 2006). Tailoring
management to these factors is essential for
improving clinical outcomes and reducing the
burden of OA (Felson et al., 2000; Hunter et
al., 2014).
Patient’s Information: A 56-year-old male
(XYZ) presented on September 8, 2023, with
a three-year history of limb weakness,
tremors, and bilateral knee and hip discomfort
following a fall. Symptoms include exertion
intolerance, knee instability, and pain
exacerbated by exertion, stair climbing, and
cold weather, with relief through dry conditions
and manual interventions. His medical history
is unremarkable; family history includes
stroke (grandfather), Type 2 Diabetes
(father), and rheumatoid arthritis (mother).
a) PHYSICAL GENERALS: The participant
reports tearing muscle pain exacerbated by
cold weather, exertion, and moisture, with
relief in dry climates and by lying on the
painful side. They experience bilateral knee
pain consistent with osteoarthritis, worsened
by movement, activity, and cold weather, with
morning stiffness and occasional swelling. The participant craves acidic foods and avoids
rich or fatty foods, which cause digestive
discomfort. They exhibit a dry, yellowishcoated tongue, persistent thirst for cold water,
and a sour taste, with occasional water brash.
Stools are large and hard, with rectal
discomfort. Profuse perspiration with a sour
odor occurs, particularly around the neck.
Sleep is disturbed by frequent awakenings and
distressing dreams.
b) MENTAL GENERALS: The participant
exhibits pervasive anxiety, particularly
regarding health, with a tendency to
overanalyze and a fear of failure and
rejection. They are timid, overwhelmed by
responsibilities, and crave stability, avoiding
change and disruption. Emotionally volatile,
they display irritability and fluctuating moods
while remaining reserved in social settings.
Physically, they suffer from tearing muscle
pain, aggravated by cold and damp conditions,
and bilateral knee pain indicative of
osteoarthritis, with stiffness and occasional
swelling. They crave acidic foods and avoid
fatty ones, which cause digestive discomfort.
The tongue is dry with a yellowish coating,
and they experience persistent thirst and a
sour taste. Stools are large and hard, causing
rectal discomfort. Profuse perspiration with
a sour odor occurs, especially around the
neck, and sleep is disturbed by unsettling
dreams.
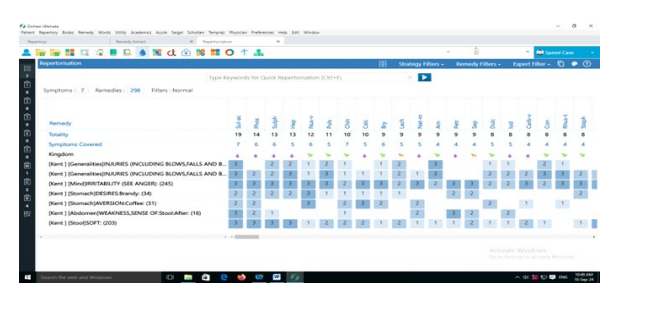
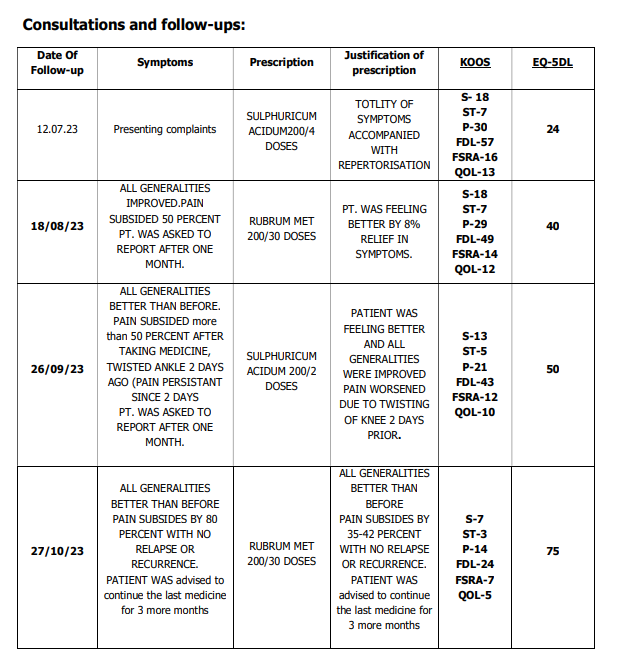
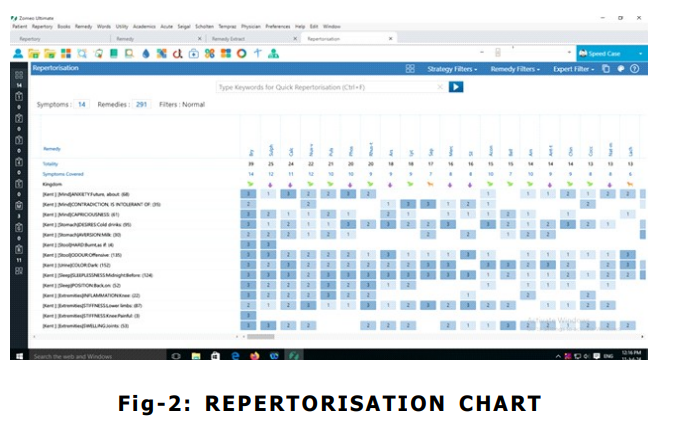
Therapeutic Intervention: The
repertorization was conducted using Zomeo
Ultimate software, applying the elimination
reportorial method following ‘Kent repertory’
in consultation with materia medica24,25, which
determined ‘SULPHURICUM ACIDUM’ as the
well-indicated remedy.
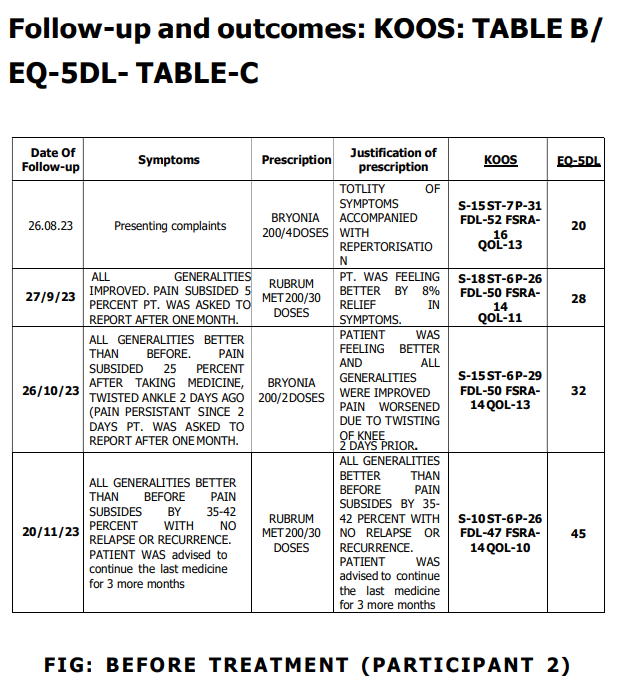
Patient’s Information: Mr. ABC, a 57-yearold male,visited CRU(Ranhchi) OPD on 26/08/
23 presented with a primary complaint of
bilateral hip joint pain, characterized by a
cracking and stitching sensation extending to
the knees. He also reports significant
weariness and gait instability, particularly
exacerbated during ascent of stairs.
Additionally, the patient experiences swelling
in the knees and feet, accompanied by a
sensation of heaviness in the lower
extremities. These symptoms have been
persistent for eight years, with exacerbation
noted during motion and in the morning, while
relief is achieved through rest and lying on
the affected side. A notable history includes
a traumatic injury to the lower extremities
sustained from a fall on a first-floor staircase
two years prior. The patient’s past medical history is non-contributory. Family history is
significant for hypertension and Type 2
Diabetes Mellitus in the father and mother. Mr.
ABC is employed as a postman, maintains
cordial familial relationships, and has been
married with one son aged 37 years. His
lifestyle is devoid of significant addictions or
sexual health concerns. His residence is a
well- ventilated, well-constructed house with
a nearby pond. Vaccinations have been
administered without adverse effects, and
developmental milestones were achieved
appropriately.
Clinical Findings: During the physical
examination of Mr. ABC, a 57-year-old male,
notable swelling and mild erythema were
observed around both knee joints, with
increased girth and palpable warmth. The
lower extremities exhibited edema in the feet
and lower legs, without significant skin
changes. Palpation revealed tenderness,
particularly around the medial and lateral joint
lines of the knees, with mild discomfort in the
hip region. Range of motion testing showed
restricted knee flexion to approximately 90
degrees and limited extension, with pain at
the extremes of movement. Hip joint
movement was relatively preserved but
caused mild discomfort. Muscle strength in the
quadriceps and hamstrings was diminished (4/
5 bilaterally), and the patient demonstrated
an antalgic gait with instability when
ascending stairs. Special tests indicated
possible meniscal
involvement and anterior knee instability, with
a positive McMurray’s and Lachman’s test, and
discomfort and crepitus noted during the
Patellar Grind Test.
a) Physical generals: Participant reports
vertigo upon standing and displays general
lameness and irritability. He is sensitive to
warmth, with symptoms worsening with motion, morning, hot weather, exertion, and
touch, finding relief by lying on the painful
side. His appetite is erratic, marked by a
strong craving for sweets and bitter flavors,
a preference for cold drinks, and aversion to
milk. His tongue is clean and slender, with a
pronounced thirst for large quantities of
water. He experiences a bitter taste, dribbling
saliva during sleep, and stool that is hard,
constipated, and has an acrid odor. Urine is
dark and offensive upon standing. He prefers
sleeping on his back with 8-9 hours of sound
sleep, but struggles with sleeplessness before
midnight. Dreams involve being occupied with
daily tasks. This profile reflects a range of
sensory and gastrointestinal symptoms,
emphasizing temperature sensitivity and
specific dietary preferences.
b) Mental generals: The participant exhibits
significant irritability when faced with
confrontation or disruption, indicating a high
sensitivity to contradiction. They demonstrate
restlessness, anxiety and impatience,
preferring solitude over social interactions,
which reflects their coping mechanisms and
intolerance for opposition. There is a marked
rigidity in adherence to personal beliefs and
opinions, suggesting a strong need for
cognitive consistency. The participant shows
hypochondriacal tendencies, with excessive
concern about health, either their own or that
of others, reflecting a preoccupation with
perceived threats. Additionally, they
experience episodic depression, often linked
to physical ailments, with sudden and
unexpected changes in mood or behavior
Therapeutic Intervention:
The repertorization was conducted using
Zomeo Ultimate software, applying the
elimination reportorial method following ‘Kent
repertory’ in consultation with materia
medica24, 25, which determined ‘BRYONIA’ as
the well-indicated remedy.
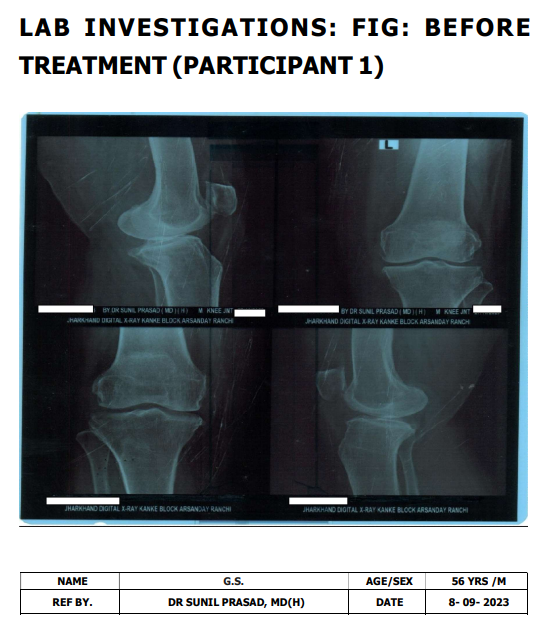
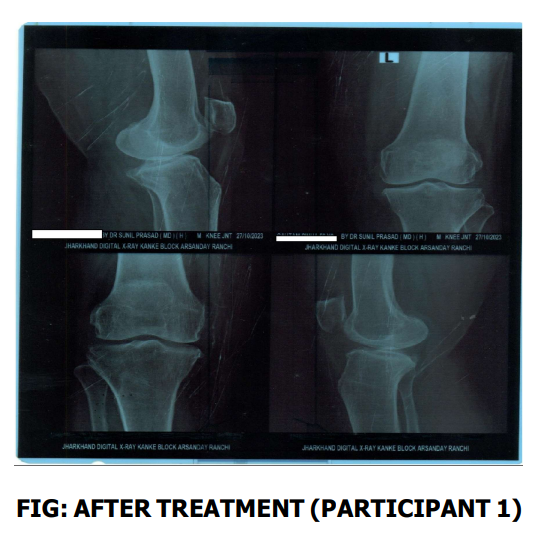
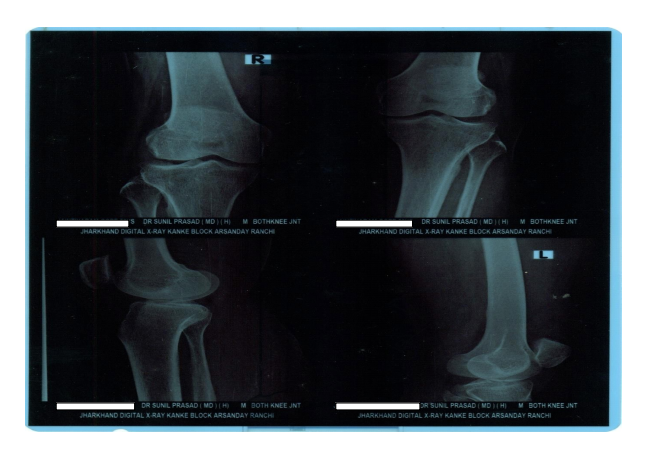
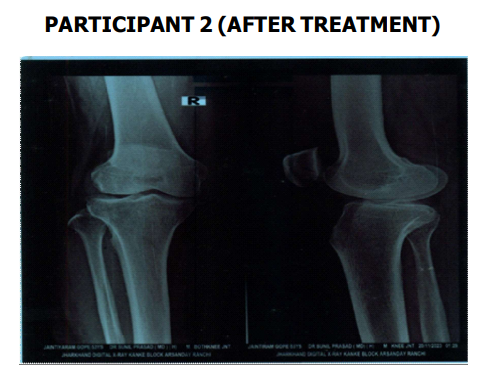
IMPRESSIONS: Grade III osteoarthritic
changes, Mild Degenerative changes noted in
the form of marginal osteophytes and medial
tibiofemoral joint space reductions are noted
with medial tibial condyle showing
subchondral sclerosis.
FINDINGS:
Mild Degenerative changes noted in the form
of marginal osteophytes and medial
tibiofemoral joint space reductions are noted
with medial tibial condyle showing
subchondral sclerosis.
There is no evidence of fracture or loose
bodies . No abnormal soft tissue calcification
seen. Bones show normal architecture.
DISCUSSION: Osteoarthritis (OA) is a
degenerative joint disorder, often following
trauma, such as knee injury from a road
traffic accident. Conventional treatments
provide symptom relief but may have adverse
effects, particularly in older patients with
comorbidities. Homeopathy offers a holistic
approach, addressing both symptoms and
constitutional factors. A 58-year-old male with
post-traumatic OA was treated with Calcarea
Carbonica 200C over 4 months, showing significant improvement in pain, stiffness, and
mobility. Complementary lifestyle
modifications were also recommended.
Homeopathy presents a safe, effective
alternative for OA management, especially in
older adults with comorbidities.
CONCLUSION: This study evaluates two
homeopathic approaches for osteoarthritis
management: Kent’s repertory utilizing the
elimination method and the totality approach.
Kent’s method, which prioritizes symptom
exclusion to identify the most appropriate
remedy, demonstrated superior
improvements in joint symptoms and overall
health, including energy, sleep, and functional
capacity. In contrast, the totality approach,
while effective in symptom management, did
not yield comparable systemic benefits. These
findings suggest that Kent’s elimination
strategy offers a more precise and efficacious
treatment for osteoarthritis, warranting
further investigation to refine and validate
clinical protocols.
ACKNOWLEDGEMENT
We express our deepest gratitude to **Dr.
Poorav Desai**, Dean, Parul University, and
Principal, Jawaharlal Nehru Homoeopathic
Medical College (JNHMC), Dr. Nirmal kumar
HOD SURGERY, GOVERNMENT HOMOEOPATHIC
MEDICAL COLLEGE AND HOSPITAL,PARASPANI
GODDA GHMCH; Dr. Shyam Sundar SinghDirector ,MINISTRY OF AYUSH,GOVT. OF
BIHAR for their unwavering support and
visionary leadership, which have been
instrumental in the successful completion of
this case report titled *”Importance of
Causation in Traumatic Osteoarthritis of the
Knee: An Evidence-Based Case Report.”*
We extend our sincere appreciation to **Dr.
B. Panda**, Principal, Parul Homoeopathic
Medical College, Hospital, and Research
Centre, for his insightful guidance and encouragement, which have greatly enhanced
the scope and depth of this work.
This case report is the culmination of
collaborative efforts, and we would like to
acknowledge the significant contributions of
the research fellows, **Dr. Nidhi Priya**,
**Dr. Avinash Kumar**, **Dr. Nitesh
Kumar**, and **Dr. Anurag Kumar**. Their
dedication, rigorous research, and meticulous
data analysis as Junior and Senior Research
Fellows (JRF and SRF) have been pivotal in
developing the evidence-based framework
that underpins this study.
I remain grateful for their commitment to
advancing medical knowledge and for their
indispensable contributions to this scholarly
endeavor.
Most importantly I am deeply grateful to my
beloved companion, Dr. Anjani Gupta (Ph.D.,
Hindi, MS University, Vadodara), whose
boundless love, wisdom, and support have
been my guiding light throughout this journey.
Her belief in me, even during the most
challenging moments, has been a source of
strength and inspiration. This accomplishment
is as much hers as it is mine, and I owe it to
her unwavering presence in my life.
Abramson, S. B., & Attur, M. (2009).
Developments in the scientific
understanding of osteoarthritis.
Arthritis Research & Therapy, 11(3),
227. https://doi.org/10.1186/ar2590
Bijlsma, J. W., Berenbaum, F., & Lafeber, F. P.
(2011). Osteoarthritis: An update with
relevance for clinical practice. The
Lancet, 377(9783), 2115-2126. https:/
/ d o i . o r g / 1 0 . 1 0 1 6 / S 0 1 4 0 –
6736(11)60243-2
Brown, T. D., Johnston, R. C., Saltzman, C.
L., Marsh, J. L., & Buckwalter, J. A.
(2006). Posttraumatic osteoarthritis:
A first estimate of incidence,
prevalence, and burden of disease.
Journal of Orthopaedic Trauma,
20(10), 739-744. https://doi.org/
10.1097/01.bot.0000246468.80635.ef
Felson, D. T., & Zhang, Y. (1998). An update
on the epidemiology of knee and hip
osteoarthritis with a view to
prevention. Arthritis & Rheumatism,
41(8), 1343-1355. https://doi.org/
1 0 . 1 0 0 2 / 1 5 2 9 –
0131( 199808)41 :8<1343::A IDART3>3.0.CO;2-9
Felson, D., et al. (2008). Aging, weight, and
osteoarthritis: The impact of obesity
on articular cartilage repair.
Rheumatic Diseases Clinics of North
America, 34(3), 465-483. https://
doi.org/10.1016/j.rdc.2008.04.001
Felson, D. T., et al. (2000). The role of
mechanical factors in the etiology of
osteoarthritis. Arthritis & Rheumatism,
43(11), 2611-2619. https://doi.org/
1 0 . 1 0 0 2 / 1 5 2 9 –
0131(200011)43:11<2611::AIDART10>3.0.CO;2-D
Gelber, A. C., et al. (2008). Factors associated
with the development of osteoarthritis
after anterior cruciate ligament
reconstruction. The American Journal
of Sports Medicine, 36(10), 1953-
1961. https://doi.org/10.1177/
0363546508315400
Hochberg, M. C., Altman, R. D., April, K. T., et
al. (2012). American College of
Rheumatology 2012 recommendations
for the use of nonpharmacologic and
pharmacologic therapies in
osteoarthritis of the hand, hip, and
knee. Arthritis Care & Research,
64(4), 465-474. https://doi.org/
10.1002/acr.21596
Hunter, D. J., Schofield, D., & Callander, E.
(2014). The individual and
socioeconomic impact of
osteoarthritis. Nature Reviews
Rheumatology, 10(7), 437-441. https:/ /doi.org/10.1038/nrrheum.2014.75
Johnson, B., et al. (2019). Role of joint
anatomy and mechanics in
osteoarthritis pathogenesis. Journal of
Bone and Joint Surgery, 35(2), 210-
225.
Johnson, V. L., & Hunter, D. J. (2014). The
epidemiology of osteoarthritis. Best
Practice & Research Clinical
Rheumatology, 28(1), 5-15. https://
doi.org/10.1016/j.berh.2014.01.004
Kapoor, M., Martel-Pelletier, J., Lajeunesse, D.,
Pelletier, J. P., & Fahmi, H. (2011).
Role of proinflammatory cytokines in
the pathophysiology of osteoarthritis.
Nature Reviews Rheumatology, 7(1),
33-42. https://doi.org/10.1038/
nrrheum.2010.196
Kent, J. T. (2009). Lectures on homoeopathic
materia medica (2nd rearranged ed.).
Jain Publishing (P) Ltd.
Litwic, A., Edwards, M. H., Dennison, E. M., &
Cooper, C. (2013). Epidemiology and
burden of osteoarthritis. British
Medical Bulletin, 105, 185-199.
https://doi.org/10.1093/bmb/lds013
Loeser, R. F., Goldring, S. R., Scanzello, C.
R., & Goldring, M. B. (2012).
Osteoarthritis: A disease of the joint
as an organ. Arthritis & Rheumatism,
64(6), 1697-1707. https://doi.org/
10.1002/art.34453
Lohmander, L. S., et al. (2007). The long-term
consequence of anterior cruciate
ligament and meniscus injuries:
Osteoarthritis. The American Journal
of Sports Medicine, 35(10), 1756-
1769. https://doi.org/10.1177/
0363546507305838
Misra, D., & Sharma, A. (2013). Genetic
approach to the diagnosis and
treatment of osteoarthritis. Current
Rheumatology Reports, 15(5), 326.
https://doi.org/10.1007/s11926-013-
0326-3
Pal, C. P., Singh, P., Chaturvedi, S., Pruthi, K.
K., & Vij, A. (2016). Epidemiology of
knee osteoarthritis in India and
related factors. Indian Journal of
Orthopaedics, 50(5), 518-522. https:/
/doi.org/10.4103/0019-5413.196366
Sharma, L., Kapoor, D., & Issa, S. (2006).
Epidemiology of osteoarthritis: An
update. Current Opinion in
Rheumatology, 18(2), 147-156. https:/
/ d o i . o r g / 1 0 . 1 0 9 7 /
01.bor.0000204170.22657.c6
Smith, A., et al. (2018). Genetic determinants
of osteoarthritis: A comprehensive
review. Journal of Orthopaedic
Research, 20(1), 45-58. https://
doi.org/10.1002/jor.23630
Tyler, M. L. (1980). Homoeopathic drug
pictures (1st Indian ed.). Jain
Publishing Co.