Indian Journal of Health Social Work
(UGC Care List Journal)
PROBLEMS OF PEOPLE LIVING WITH HIV: A CASE STUDY OF
MANIPUR
Wahenbam Ranbir Singh
Medical Social Worker, Community Medicine Department, Regional Institute of Medical
Sciences, Imphal
Correspondence: Wahenbam Ranbir Singh, email: w.ranbir@gmail.com
ABSTRACT
Keywords: Discrimination, Marital conflict, Counsellor
INTRODUCTION
HIV (Human Immunodeficiency Virus) is a lifelong contagious viral disease that weakens the individual’s immune system without treatment and progresses to the life threatening illness known as AIDS (acquired i mmunodeficiency syndrome). The t ransmission of HIV continues to be designated as a global epidemic by World Health Organisation. Globally, the incidence of people living with HIV (PLHIV) was 38.4 million (33.9-43.8 million), with an expected 650000 (510000-860000) mortality from the disease by 2021. Despite substantial developments in antiretroviral therapy supply, and access, as well as a rapid growth of awareness efforts over the past thirty years, almost 2 million each year cases of infections have been documented (UNAIDS,2023; WHO, 2022). In 2019, HIV infection resulted in 47.63 million. Disability Adjusted Life Years (DALYs) worldwide, a 1.28-fold increase over 1990 (UN, 2015). This poses significant hurdles in meeting the 2030 Sustainable Development Goal 3 objectives of promoting good health and well-being for everyone (UNAIDS, 2020; Warren et al., 2017) and their vow to ‘Ending the AIDS epidemic as a public health issue’ (SGD-3, Target 3.3) (Zeng et al, 2016). India has the world’s third highest overall HIV burden, with an anticipated 2.3 million PLHIV in 2021, 63 thousand of whom were recently i nfected, and 42 thousand yearly reported fatalities due to the disease. Additionally, only 77% of PLHIV were conscious of their diagnosis, and only 65% had begun ART medication (UNAIDS, 2022). HIV/AIDS has a substantial adverse impact on health, social, and economic growth in an emerging lower middle-income country like India. Since 1992, the government of India, under the Ministry of Health and Family Welfare (MoHFW) has launched the National AIDS Control Organization (NACO) in order to regulate and prevent the further spread AIDS epidemic in India. It has accomplished major achievements in reducing the yearly prevalence of fresh infections with HIV by two thirds and the death rate by more than half (54%) over the last two decades (NACO, 2015). Moreover, the country’s prevalence has consistently decreased from 0.54% in 2000 2001 to 0.22% in 2020 (NACO, 2022a). Although the general prevalence is reasonable, there is substantial variation among states, with higher levels in Mizoram, Nagaland, and Manipur. Other states and union territories with adult rates of HIV exceeding the national average are Andhra Pradesh, Meghalaya, Telangana, Karnataka, Delhi, Maharashtra, Puducherry, Punjab, Goa, and Tamil Nadu (NACO, 2022b). These considerable inter-state variances highlight the importance for faster and extensive preventative measures to reduce population risk by up to 80% by 2025 (NACO, 2020).The HIV/AIDS epidemic in India is highly heterogeneous, which influences population transmission dynamics and the burden of epidemiological disease. High-risk categories include female sex workers (FSWs), men having sex with men (MSMs), injectable drug users (IDUs), truckers, low socioeconomic status (SES) populations, and migrants, among others. As a result, HIV risk is an outcome of adverse social variables that contribute to current high-risk behavior and low knowledge (Shrivastava et al., 2019; Kefale et al., 2020). Aside from the physiological concerns among the individuals with HIV/AIDS encounter, social and psychological issues are also regarded as significant hurdles (Stangl, et al., 2013). Stigmatization and prejudice, in particular, are substantial hurdles to HIV/AIDS infected individual’s access to healthcare services and testing, as well as their treatment adherence (Katz et al., 2013). Thus, researching the extent of stigma and discrimination against people with HIV/AIDS is regarded as one of the foremost emphasis for HIV/AIDS studies (Tran, et al., 2019; Greenwood et al., 2021). The detrimental impact of negative perceptions toward HIV/AIDS infected people can hinder strategies to regulate and prevent the disease (Vorasane et al, 2017; Rintamaki et al., 2019). Furthermore, the potential implications of HIV stigma include a lack of desire to share HIV status, a poor influence on health seeking behavior, and an adverse effect on the necessary social support (Brown et al., 2003; Vanable et al., 2006). Manipur, which covers around 22,327 km2 and has a population of 2.7 million residents (a population density of 120 individuals per square kilometer), has been estimated to be one of India’s most affected centers of the worldwide epidemic of HIV/AIDS. Manipur, a distant north-eastern corner of the country with only 0.2% of the overall population, accounts for roughly 8% of India’s total HIV positive patients. The prevalence of HIV rates among IDUs climbed dramatically, from 2% to 3% in 1989 to more than 50% in 1991 and 64% in 2000 (Saha MK et al., 2000). The magnitude of the HIV/AIDS pandemic continues a challenge for the state. HIV/AIDS has been recognized as an alarming public health concern, and controlling its spread appears to be a formidable challenge. In contrast to other states in India, the spread of HIV in this region is mostly linked to the exchange of HIV-infected injecting equipment/ needles across Injecting Drug User (IDUs) (Narain JP et al., 1994). IDUs are an easy target for transmitting HIV. While the epidemic was first documented among IDUs, HIV is no longer limited to IDUs and is now starting to surface in the general population. Due to the lack of curative treatment or vaccines, public awareness of HIV/AIDS should be the foundation for managing the epidemic (Yadav et al., 2016). Earlier research has revealed that a lack of precise and complete understanding of HIV, particularly about the modalities of virus transmission, is a major cause of incident HIV infections (Nubed & Akoachere, 2016; Janahi et al., 2016). However, knowledge alone cannot prevent infection; practice is required to get the desired results (Teshome et al., 2016). In order to develop successful educational and awareness programs to tackle this important public health concern, it is critical to examine the problem of HIV/AIDS in state of Manipur.
The primary objective of the study is to assess the consequence/issues faced by the PLHIV in the context of Manipur.
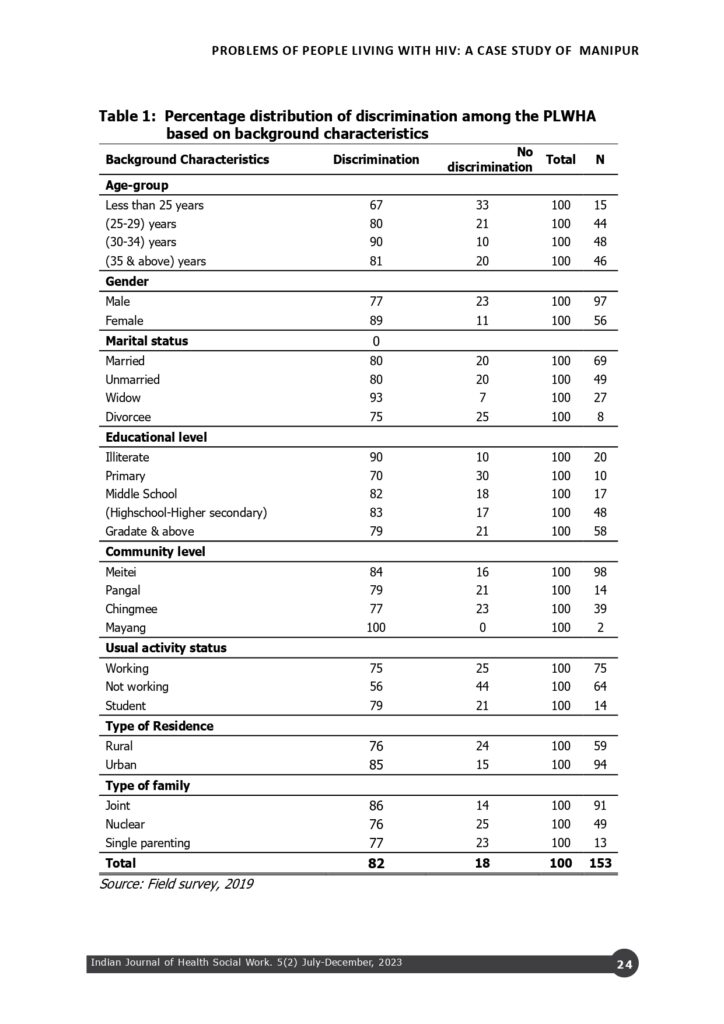
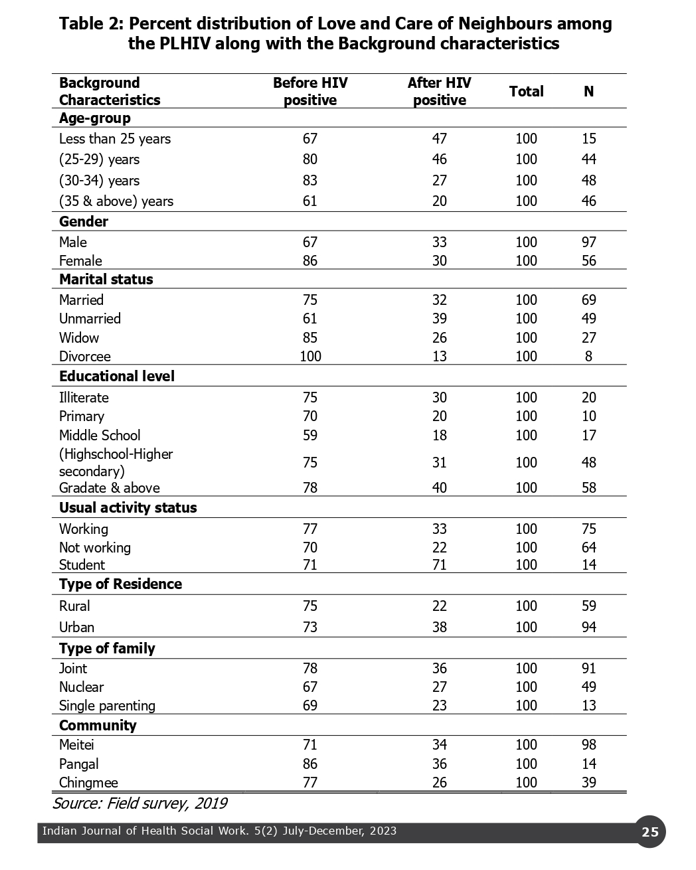
The paper is a cross-section study with purposive in nature. The primary data were collected in 2019 in some districts (Imphal East, Imphal West, Thoubal & Churchandpur) of Manipur. With their consent, altogether 153 patients living with HIV (PLHIV) in Manipur were collected along with their various socioeconomic and demographic variables such as age, gender, marital status, types of community, educational level of the individuals, employment status, types of f amily and type of residence. Other characteristics such as discrimination, love and care by neighbours and marital conflict were also collected in the survey. Further, some case studies with unique in nature experienced by PLHIV were also accessed for proper understanding of the research study.
Table-1 describes the discrimination faced by the PLHIV and as data suggest discrimination is more among the older persons compared to the youngest in the age less than 25 years but the level is not consistent. This pattern is similar in case of marital status. The illiterate persons had a higher level of discrimination compared to the higher educated. The urban people had a higher level of discrimination compared to the persons living in the rural areas. However, it can also be noticed that when the people are from the joint family and working happened to have higher level of discrimination. Though it is not very accurate they are the perceived the discrimination that they faced in their life.

Case study -I Rani, 24, a widow of injecting drug user (IDUs) is from Thoubal district. She studied class X and got married. Her husband held an M.A. in English and was employed in a private school. Before marriage, she was unaware of her husband’s drug behaviour. However, he became addicted to substances during his post-graduate years as well. She discovered her HIV status in the routine antenatal check-up. She was counselled and convinced of having HIV test since her husband was already HIV+. Ultimately, Rani also found herself HIV+. She gave birth to a baby and soon after that she along with her husband joined Manipur Network of Positive People (MNP+) an NGO worked for the PLHIV in Manipur. After joining MNP+ she got training to handle the situation. Rani retorted that nobody was looking after her when she fell ill at her in-law’s house only to get the ill treatment. She was refused to get any resource for her treatment from her in-laws and she also hid her situation from her parents even. She was even denied of attending the last rite of her husband after he died. She was of the opinion that majority of women in her situation faced such kind of discrimination in almost every part of the state.
From the cases it becomes clear that HIV is a condition of highly deplorable. The first case shows the condition of being a PLHIV woman who suffered both from the husband being a liar and family not considering the situation faced by women as a group in Manipur. Afterall her natal family stood by her and extended the help which she needed most at the time of need. The second case was the experience of a youth who tasted drugs in the early age. Because of his misadventure he ended up without having nothing from his academic life and a result his family left him unattended while he devoted his life to the cause of HIV/ AIDS. The third case is also a transmission from the unsuspecting husband who was away from home for a long time in service. The unguarded moments of life of the husband put Hoinu into the dreaded situation and led her to the world of HIV. She was devastated but she carried on her life for the sake of her small innocent children. Her message to us is to avoid sexual relationships with strangers, as well as using illicit drugs and other dangerous behaviour.
The current paper focuses solely on the perceptions and experiences of people living with HIV (PLHIV), providing a boost and direction for future research that examines the perceptions and experiences of general population (non-PLHIV) in tailoring more effective measures to improve the quality of life of PLHIV. In short, the research paper was able to emphasize the stigma and discrimination experienced by PLHIV in the state of Manipur. It was able to address the fact that women (PLHIV) are more vulnerable to discrimination and marital turmoil. The finding furnished deep understanding of the problem which needs valuable intervention through social support, professional social workers, ASHA and others community-based health worker to improve the quality of life for PLHIV in Manipur.
REFERENCES
Brown, L.; Macintyre, K.; Trujillo, L (2003).
Interventions to reduce HIV/AIDS
stigma: What have we learned? AIDS
Educ. Prev. 15, 49–69.
Greenwood, G.L.; Wilson, A.; Bansal, G.P.;
Barnhart, C.; Barr, E.; Berzon, R.;
Boyce, C.A.; Elwood, W.; Gamble
George, J.; Glenshaw, M.; et al.,
(2021). HIV-Related Stigma Research
as a Priority at the National Institutes
of Health. AIDS Behav. 1–22.
Janahi ,E.M.; Mustafa, S.; Alsari S.; Al
Mannai, M.; Farhat, G.N. (2016).
Public knowledge, perceptions, and
attitudes towards HIV/ AIDS in
Bahrain: a cross-sectional study. The
Journal of Infection in Developing
Countries. 10(09):1003-1011.
doi:10.3855/jidc.7665.
Joint United Nations Programme on HIV/AIDS
((2023). Global HIV & AIDS statistics- fact sheet. UNAIDS. https://
www.unaids.org/en/resources/fact
sheet
.
Joint United Nations Programme on HIV/AIDS.
India. UNAIDS (2022). https://
www.unaids.org/en/regionscountries/
countries/india
.
Katz, I.T.; Ryu, A.E.; Onuegbu, A.G.; Psaros,
C.; Weiser, S.D.; Bangsberg, D.R.;
Tsai, A.C. (2013). Impact of HIV
related stigma on treatment
adherence: Systematic review and
meta-synthesis. Journal of the
International AIDS Society. 16 (Suppl.
2), 18640.
Kefale B, Damtie Y, Yalew M, Adane B,
Arefaynie M. (2020). Predictors of
comprehensive knowledge of HIV/AIDS
among people aged 15–49 years in
Ethiopia: a multilevel analysis. HIV
AIDS (Auckl). 12:449-456.
Narain, J.P. (1994). Risk factors for HIV
transmission in India. AIDS (London,
England) 8, S77–S82.
National AIDS Control Organisation (2015).
Part-B National AIDS Control
Organisation. NACO. https://
naco.gov.in/sites/default/files/
annual_report%20_NACO_2014
15_0.pdf.
National AIDS Control Organisation (2020). Sankalak: Status of National AIDS
Response. NACO.
National AIDS Control Organisation (2022).
Part-B National AIDS Control
Organisation.NACO.https://
naco.gov.in/sites/default/files.
Nubed. C.K & Akoachere, J.T.K. (2016).
Knowledge, attitudes and practices
regarding HIV/AIDS among senior
secondary school students in Fako
Division, South West Region,
Cameroon. BMC Public Health. 16(1).
Rintamaki, L.; Kosenko, K.; Hogan, T.; Scott,
A.M.; Dobmeier, C.; Tingue, E.; Peek,
D. (2019). The Role of Stigma
Management in HIV Treatment
Adherence. International Journal of
Environmental Research and Public
Health, 16, 5003.
Saha, M.K.(2000). Prevalence of HCV & HBV
infection amongst HIV seropositive
intravenous drug users & their non
injecting wives in Manipur, India.
Indian Journal of Medical Research.
111, 37–39.
Shrivastava, S.; Shrivastava, P.; Ramasamy,
J. (2019). Challenges in HIV care:
Accelerating the pace of HIV-related
services to accomplish the set global
targets. Annals of Tropical Medicine
and Public Health. 10(3).
Stangl, A.L.; Lloyd, J.K.; Brady, L.M.; Holland,
C.E.; Baral, S. (2013). A systematic
review of interventions to reduce HIV
related stigma and discrimination from
2002 to 2013: How far have we come?
International Journal of Environmental
Research and Public Health, 16, 2;
18734.
Teshome, R.; Youjie ,W.; Siraj, N. (2016).
Comparison and association of
comprehensive HIV/AIDS knowledge
and attitude towards people living
with HIV/AIDS among women aged 15
49 in three East African Countries:
Burundi, Ethiopia and Kenya. Journal
of AIDS & Clinical Research. 7(4).
doi:10.4172/2155-6113.1000559
Tran, B.X.; Phan, H.T.; Latkin, C.A.; Nguyen,
H.L.T.; Hoang, C.L.; Ho, C.S.H.; Ho,
R.C.M. (2019). Understanding Global
HIV Stigma and Discrimination: Are
Contextual Factors Sufficiently
Studied? (GAP(RESEARCH)). Int. J.
Environ. Res. Public Health. 16, 1899.
UNAIDS (2020). Joint United Nations
Programme on HIV/AIDS. 90–90–90:
good progress, but the world is off
track for hitting the 2020 targets.
https://www.
unaids.org/en/
resources/presscentre/featurestories/
2020/september/20200921_90-90-90.
United Nations (2015). Transforming our
world: The 2030 agenda for
sustainable development. UN. https:/
/sdgs.un.org/2030agenda
.
Vanable, P.A.; Carey, M.P.; Blair, D.C.;
Littlewood, R.A (2006). Impact of HIV
related stigma on health behaviors
and psychological adjustment among
HIV-positive men and women. AIDS
Behavioral. 10, 473–482.
Vorasane, S.; Jimba, M.; Kikuchi, K.; Yasuoka,
J.; Nanishi, K.; Durham, J.; Sychareun,
V. (2017). An investigation of
stigmatizing attitudes towards people
living with HIV/AIDS by doctors and
nurses in Vientiane, Lao PDR. BMC
Health Service Research, 17, 125.
Warren, C.E.;Hopkins, J; Narasimhan, M.
Collins, L.; Askew, I.; Mayhew, S.H.
(2017). Health systems and the SDGs:
lessons from a joint HIV and sexual
and reproductive health and rights
response. Health Policy Plan. 33,
4;102- 107.
World Health Organization. HIV. WHO; (2022).
https://www.who.int/news-room/
fact-sheets/detail/hiv-aids
.
Yadav, J., Gautam, S., Singh, K. (2016). Differential in awareness and
comprehensive knowledge of HIV/AIDS
and its determinants among youth in
India: a population based cross
sectional
study.
American
International Journal of Research in
Humanities, Arts and Social Sciences.
222-230.
Zeng, W.; Shepard, D.S.; Avila-Figueroa, C.;
Ahn, H. (2016). Resource needs and
gap analysis in achieving universal
access to HIV/AIDS services: a data
envelopment analysis of 45 countries.
Health Policy and Planning, 31(5):624
633.
Conflict of interest: None
Role of funding source: None