Indian Journal of Health Social Work
(UGC Care List Journal)
QUALITY OF LIFE AMONG PARENTS OF CHILDREN WITH TYPE 1
DIABETES MELLITUS
Jayachandran M R1 & Laxmi2
1Medical Social Service Officer, All India Institute of Medical Sciences, Bhubaneswar,
2Assistant Professor, Department of Social Work, Central University of Kerala,
Correspondence: Jayachandran M R, e-mail: msso_jayachandran@aiimsbhubaneswar.edu.in
ABSTRACT
Background: The quality of life is considered exceptionally imperative for the family of children
with unremitting infection. Parents have a critical part in choosing the quality of life among
families of children with chronic illnesses. Aim: The study aims to assess the level of quality of
life and to measure the socio-demographic profile among parents of children with type 1 diabetes
mellitus. Methods and Materials: The study used an Explanatory research design, and
quantitative data collection was employed in this study. Results: The results of the current
study showed that parents of children with type 1 diabetes mellitus reported higher levels of
quality of life in the physical, social, and environmental domains. When compared to other quality
of life domains, the psychological quality of life domain has demonstrated a lower quality of life.
Conclusion: The findings of this study will assist various stakeholders, including policymakers,
medical professionals, medical social workers, mental health specialists, and researchers, in
comprehending the challenges faced by parents and caregivers.
Keywords: Quality of Life, Chronic illness, Diabetes Mellitus, Parents, Children.
INTRODUCTION
A person’s or a community’s overall state of
well-being is regarded as their quality of life,
and health-related studies typically assess life
quality (Sathyananda & Manjunath, 2017).
According to the World Health Organization,
quality of life means “Individuals’ perception
of their position in life in the context of the
culture and value systems in which they live
and in relation to their goals, expectations,
standards and concerns. It is a broad-ranging
concept affected in a complex way by the
persons’ physical health, psychological state,
level of independence, social relationships,
and their relationship to salient features of
their environment’’ (The WHOQOL Group,
1995, p.1403). The World Health Organization
has defined four domains of measuring quality
of life, which are physical, psychological, social
relationships, and environmental factors.
Physical health refers to human functions such
as daily life, sleep, work capacity, rest,
energy, discomfort, weakness, and
medication. Psychological health includes an
individual’s thinking, feelings, appearance,
mental background, focus, and self
confidence. Social relationship creates
individual support systems, sexual needs, and
relationships with others. Environmental
factors include an individual’s ability to
appreciate freedom, the economy,
transportation, home and other environments,
l eisure activities, health services, skill development, and climate change (World
Health Organization, 1996). Quality of life
evaluates “an individual’s sense of wellbeing
and the degree to which he or she can
participate in the human experience” (Zhan,
1992, p. 779).
The quality of life is considered exceptionally
imperative for the family of children with
unremitting infection (Toledano-Toledano et
al., 2020; Feeley et al., 2014). Parents have
a critical part in choosing the quality of life
among families of children with chronic
illnesses (Janse et al., 2005). Appraisal of
quality of life among parents of children with
chronic illnesses is considered vital, as the
appraisal is based on the parental quality of
life, such as social, psychological, and well
being (Abreu Paiva et al., 2019). The severity
of chronic illness and the family’s financial
status are fundamental components of
parental quality of life (Siboni et al., 2019).
Children with persistent ailments directly
influence family and parental quality of life.
The parental quality of life depends on the
seriousness of the child’s illness and how
much time is spent caring for the affected
children. The parents of children with chronic
illness and their quality of life influence the
family’s social, psychological, and medical
support (Spore, 2012). Chronic diseases are
recognized to affect family circumstances
significantly and create unpleasant
circumstances. Parents’ stress may lead to
confusion, anger, time constraints, isolation,
and bitterness (Cherry, 1989). When the child
features a persistent ailment, diverse
variables such as social, mental, physical, and
monetary stability influence the parent’s
quality of life (Zhang, Wei, Shenand, and
Zhang, 2015). Chronic illness is considered a
challenging circumstance for families; the
child’s sickness impacts everyday activities.
Great quality of life is fundamental for these
families (Amirian et al., 2017). Children with
l ong-term persistent conditions have
adversely influenced their parents quality of
life (Witt et al., 2010). Type 1 diabetes mellitus
is considered a disease and needs lifelong
medical treatment (Vehik et al., 2007).
Type 1 diabetes mellitus is considered
childhood diabetes, but it can occur in people
of any age. Currently, there is no vaccine to
prevent this disease. A person with type 1
diabetes can live a healthy life, but they need
diabetes test equipment, continuous insulin
hormone, diabetes education, and social
support. Type 1 diabetes is caused by an
autoimmune problem and affects the immune
system of the beta cells of the pancreas, which
produce the insulin hormone in the human
body. In this case, the pancreas does not
produce enough or less insulin in the human
body. The acute cause of type 1 diabetes is
unknown. Type 1 diabetes is considered a
chronic disease in childhood (Kahanovitz,
Slussand, and Russell, 2017). Parents play a
vital role in the administration of type 1
diabetes mellitus, and the parents have to give
quality well-being care to their children with
type 1 diabetes mellitus (Uhm & Kim, 2020).
Poor communication, increased family conflict,
decreased adaptation, and poor support lead
to serious issues among parents of children
with type 1 diabetes mellitus (Almeida, 1995).
The adapting techniques of parents of children
with type 1 diabetes mellitus have affected
the parental quality of life (Pierce, Kozikowski,
Lee, and Wysocki, 2017). Parents of children
with type 1 diabetes mellitus were faced with
diverse psychosocial and physical issues
related to caring for children with type 1
diabetes. Numerous responsibilities must be
fulfilled in caring for their child with type 1
diabetes (Spezia, Faulkner, & Clark, 1998).
The well-being status of children with Type 1
diabetes has impacted their parents’ quality
of life (Herbert et al., 2014). In this context,
the study aims to assess the level of quality
of life and to measure the socio-demographic
profile among parents of children with type 1 diabetes mellitus.
METHODS & MATERIALS
Explanatory research design and quantitative
data collection were employed in this study.
The convenience sampling technique was
employed to get information from
respondents. The study’s participants are
parents of children with diabetes mellitus who
are registered with Kerala’s Mittayi Project.
The Kerala state government oversees the
Mittayi Project, which aims to support children
with type 1 diabetes and their families
(Mittayi, 2017). Parents of children with type
1 diabetes mellitus are the study’s
participants, and organised interview
schedules were used to gather data from the
respondents. 338 samples in all were taken
from the Mittayi project area. The Mittayi
Project granted permission to carry out the
study. The Central University of Kerala’s
institutional human ethics committee accepted
the research.
The respondents’ socio-demographic profile
included details about the age, gender, marital
status, type of family, parents’ education,
parents’ job, and gender of the child with type
1 diabetes. The parents of children with type
1 diabetes mellitus were asked to rate their
quality of life using the World Health
Organization Quality of Life BREF (WHOQOL
BREF, 1996). The 26 statements that make up
the scale’s subdomains include environment,
social relationships, psychology, and physical
health. Based on the raw score, the WHO
quality of life BREF score was computed and
then transformed to a range of zero to one
hundred. A higher score denoted a greater
standard of living, whereas a lower score
showed a poorer standard of living (World
Health Organization, 1996).
RESULTS
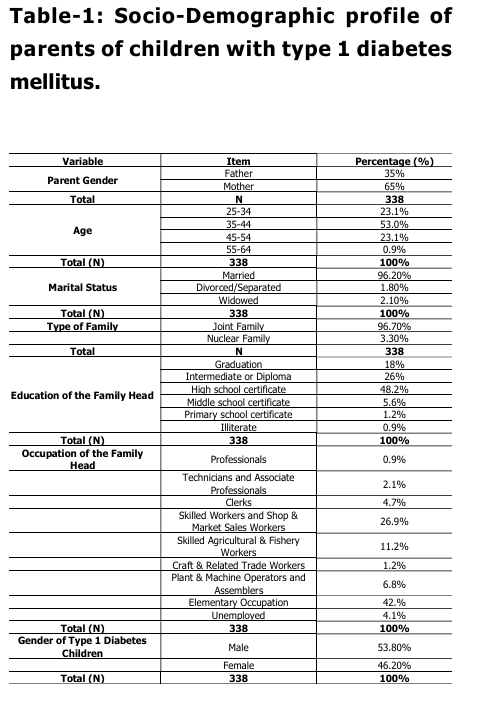
Table-1 above shows that 65 percent of
parents are female and 35 percent of parents
are male. 53 Percentage of the parents of
children with type 1 diabetes mellitus were in
the age group of 35 to 44. 23.1 percent of
parents of type 1 diabetes children belong to
the age group of 25 to 34 years. Another 23.1
percent of parents of children with type 1
diabetes mellitus were in the age group of 45
to 54. A small proportion (0.9 percent)
belongs to the 55 to 64-year age group. The
marital status: 96.20 percent of parents of
children with diabetes mellitus were married
and living with their spouse, followed by 2.10
percent of parents who reported their marital
status as widowed, and 1.80 percent of
parents of children with diabetes mellitus
included in the study were divorced or
separated. Type of family: 96.70 percent of
parents of children with type 1 diabetes mellitus belong to the nuclear family system.
The remaining 3.30 percent of parents of type
1 diabetes children are living in the joint family
system. Parents’ Education: 48.2 percent of
parents of children with type 1 diabetes
mellitus have a high school education, and
only 0.9 percent of the parents were illiterate.
Parents Job: 42 percentage had an
elementary occupation, which was followed
by Skilled Workers and Shop & Market Sales
Workers who formed 26.9 percentage of the
total respondents, Skilled Agricultural &
Fishery Workers are 11.2% percentage, Plant
& Machine Operators and Assemblers form
6.8% percentage of total respondents, Clerks
made 4.7 percentage of the total respondents’
pool. 4.1 percent of respondents were
unemployed, Technicians and Associate
Professionals form 2.1 percent of the total
respondents, Craft & Related Trade Workers
are 1.2 percent, and professionals are 0.9
percent of the total percentage. Diabetes
Child Gender: 53.80 percent of children are
boys, and 46.20 percent of children are girls.
Figure-1: Level of Quality of Life among the
Parents of Children with Type 1 Diabetes
Mellitus.
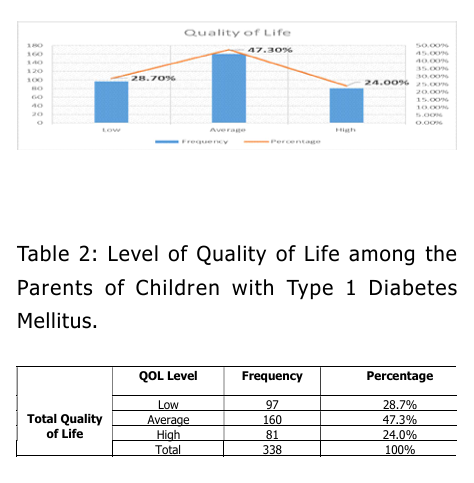
Figure-1: Level of Quality of Life among the
Parents of Children with Type 1 Diabetes
Mellitus.
The result showed the quality of life among
parents of children with type 1 diabetes
mellitus. 47.3 percent of parents of children
with type 1 diabetes mellitus reported an
average level of quality of life. 28.7 percent
of parents of children with type 1 diabetes
mellitus showed a low level of quality of life.
24 percent of parents of children with type 1
diabetes mellitus reported a high level of
quality of life.
Table 3: Descriptive statistics of quality of life
among the Parents of Children with Type 1
Diabetes Mellitus
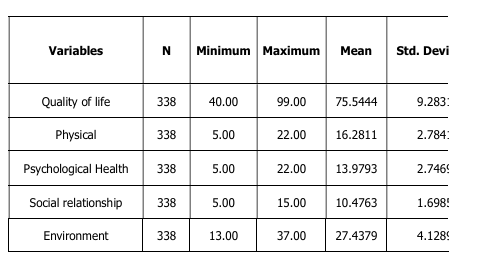
The study showed that the minimum and
maximum points of the total quality of life
were 40 and 99. The mean score of parents
of children with type 1 diabetes was 75.54,
and the standard deviation was 9.28. The
physical quality of life score showed a
minimum and maximum quality of life
composite score of 5 and 22. The mean score
of parents of children with type 1 diabetes
was 16.28, and the standard deviation was
2.78. The minimum score in the field of
psychological quality of life was 5, and the
maximum score was 22 for parents. The
mean score was 13.97, and the Std Deviation
score was 2.74. Parents of children with type
1 diabetes reported a minimum social quality
of life score of 5 and a maximum score of 15.
The mean score was 10.47, and the parental
standard deviation was 1.69. The minimum
environmental quality score of parents of
children with type 1 diabetes was 13, and the maximum score was 37. The mean score of
27.43 and standard deviation score of 4.12
showed the quality of life of the parents in
the environment.
The results of the current study showed that
parents of children with type 1 diabetes
mellitus reported higher levels of quality of
life in the physical, social, and environmental
domains. When compared to other quality of
life domains, the psychological quality of life
domain has demonstrated a lower quality of
life.
Table 4: t-test for Quality of Life among the
Parents of Children with Type 1 Diabetes
Mellitus based on Parents’ Gender
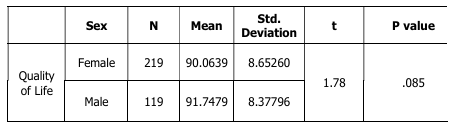
The Quality of Life among Parents of Children
with Type 1 Diabetes Mellitus: The t value
achieved is 1.78 (p>0.05), as the above table
demonstrates. At the 0.05 level of
significance, the t values are greater than the
table value of 1.96. This indicates that there
is no significant difference between the
parents of children with type 1 diabetes
mellitus who are male or female. Therefore,
i t may be said that the quality of life
experienced by male and female parents is
equal.
Table 5: ANOVA test for Quality of Life among
the Parents of Children with Type 1 Diabetes
Mellitus based on Marital Status
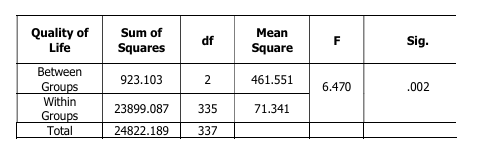
The above table describes the F value
obtained for quality of life among parents of
children with type 1 diabetes mellitus as 6.47
(p<0.05), and these F values are greater than
the table value 4.60 at the 0.05 level of
significance. That means there is a significant
difference in the Quality of Life among parents
of children with type 1 diabetes mellitus based
on the marital status of the parents. To find
out the difference among the marital statuses,
Scheffer’s post hoc test was applied for
analysis.
Table 5.1: Scheffe post hoc test Quality of Life
among the Parents of Children with Type 1
Diabetes Mellitus based on Marital Status
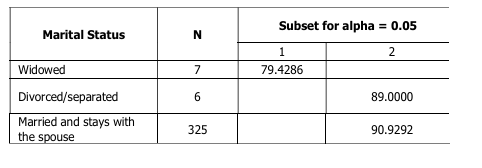
Table 7.1 indicates the Scheffe post hoc test
of quality of life based on the marital status
among parents of children with type 1
diabetes mellitus. The parents who are
married and stay with their spouse category
have reported a high mean score (57.60)
compared to other marital categories. So, it
can be concluded that there is an increased
level of Quality of Life among the parents who
live together.
DISCUSSION
The current study set out to evaluate the
quality of life for parents whose children had
been diagnosed with type 1 diabetes. type 1
diabetes mellitus is a chronic, lifelong illness.
The family is the one who has to take care of
their sick child the most. According to the
current study, parents of children with type 1
diabetes mellitus showed a marked decline
in their quality of life. According to Witt et al. (2010), parents of children with chronic
illnesses reported worsening mental health
problems and a lower quality of life for their
children. Diabetes mellitus type 1 is regarded
as a chronic condition that has an adverse
impact on the administration of health care
(Ozyazýcýoglu, Avdal and Saglam, 2017). The
primary determinants of the diabetes-related
quality of life for parents of children with type
1 diabetes mellitus have been found to be
family support and glucose management
(Hirose, Beverly and Weinger, 2012). Concerns
regarding their children’s diabetes problems
are a persistent concern for parents of
children diagnosed with type 1 diabetes
mellitus (Hilliard, Herzer, Dolan and Hood,
2011). A similar result was found in a study
by Toledano-Toledano et al., (2020) based on
the WHO Quality of Life BREF tool, which found
that 59.1 percent reported average or
average overall quality of life. and then 33.2
percent reported high overall quality of life
and 6.7 percent reported low quality of life
among parents of children with chronic
conditions. Wiedebusch, Pollmann, Siegmund,
and Muthny (2008) found moderate parental
quality of life for parents of children with
hemophilia. Spezia Faulkner and Clark
reached a similar conclusion (1998); Keklik,
Bayat and Baºdaº (2020), where the author
observes at the average quality of life of
parents of children with type 1 diabetes.
Hilliard, Herzer, Dolan, and Hood, (2011)
documented that parental care for children
with diabetes complications affected the
quality of life of parents of children with type
1 diabetes.
The results of the current study showed that
parents of children with type 1 diabetes
mellitus reported higher levels of quality of
life in the physical, social, and environmental
domains. When compared to other quality of
life domains, the psychological quality of life
domain has demonstrated a lower quality of
life. Keklik, Bayat, and Baºdaº (2020) reached
a similar conclusion about the average
psychological quality of life of parents of
children with type 1 diabetes. Mahani,
Rostami, and Nejad (2013) note that the
psychological domain of parents’ quality of life
was related to their children’s illnesses.
Delamater et al. (2001) documented that
psychosocial factors play an important role in
t he management of diabetes and in
determining the quality of life of parents.
Thorsteinsson, Loi, and Rayner (2017)
described that increasing the psychological
quality of life of parents of children with type
1 diabetes requires adequate parental social
support. The same conclusion was reached
by Yamada et al., (2012), where the author
observes that the deterioration of the quality
of life of parents related to mental health
occurred in parents of children with
developmental disorders. Koc, Bek, Vurucu,
Gokcil and Odabasi (2019) found that the
psychological health of parents of children with
epilepsy impaired quality of life and was
associated with a decrease in parental
emotional well-being. The present study’s
parents who are married and stay with their
spouse category have reported a high mean
score (57.60) compared to other marital
categories. So, it can be concluded that there
is an increased level of Quality of Life among
the parents who live together. The results of
the study conducted by Toledano-Toledano et
al. (2020) show that there is a significant
difference in the marital status and quality of
l ife of parents of children with chronic
diseases. The results of the study by Uhm and
Kim (2020) suggest a similar result, where
the authors found a significant difference in
the marital status and quality of life of parents
of children with type 1 diabetes. The same
conclusion was reached by Faulkner and Clark
(1998), who found that parents of children
living together reported a better quality of life
compared to widowed, separated, and
divorced parents. A growing body of evidence suggests that
caring for these children puts a strain on
parents. Coping with the negative
consequences of care delivery, developing and
i mplementing realistic and appropriate
response strategies is a major challenge. The
stakeholders of chronic illness should also
focus on the mental health of parents of
children with type 1 diabetes mellitus.
According to the aforementioned study
results, parents frequently perceive that
managing their child’s type 1 diabetes mellitus
has an adverse effect on their lives. The
parents are unquestionably the centre of the
family; they must not only manage the
medical concerns of their ill child but also keep
the house in order. Hence, it is the duty of
mental health specialists to take on this task
and offer care to this group that is both in
need and vulnerable. In order to give parents
of children with type 1 diabetes mellitus
greater and more targeted support and
interventions, policymakers must take these
findings into consideration.
CONCLUSION
The study found that quality of life domains
such as physical, social relationships and
environment reported improvements in quality
of life for parents of children with type 1
diabetes. The psychological domain of quality
of life showed a decrease in quality of life
compared to other domains of quality of life.
To summarize, the findings of this study will
assist various stakeholders, including
policymakers, medical professionals, medical
social workers, mental health specialists, and
researchers, in comprehending the challenges
faced by parents and caregivers. This will
facilitate the development of programmes and
i nitiatives aimed at promoting the
psychosocial well-being of parents of children
with chronic illnesses.
LIMITATIONS AND FUTURE SCOPE
This study has potential limitations. A
limitation was the use of a cross-sectional
design. The study did not take into account
the history/profile of children with type 1
diabetes, which would have helped to compare
the mental state of the parents and the health
status of the child with type 1 diabetes. In
the future, a study of parents of children with
type 1 diabetes mellitus should be conducted
on the condition of the children with a
longitudinal study design, because type 1
diabetes mellitus is identified as a lifelong
chronic illness and needs to be assessed
through the psychosocial variables from time
to time.
REFERENCES
AbreuPaiva, L. M., Gandolfi, L., Pratesi, R.,
Harumi Uenishi, R., Puppin Zandonadi,
R., Nakano, E. Y., & Pratesi, C. B.
(2019). Measuring Quality of Life in
Parents or Caregivers of Children and
Adolescents with Celiac Disease:
Development and Content Validation of
the Questionnaire. Nutrients, 11(10).
https://doi.org/10.3390/nu11102302
Almeida, C. M. (1995). Grief among parents
of children with diabetes. The
Diabetes educator, 21(6), 530–532.
h t t p s : / / d o i . o r g / 1 0 . 1 1 77 /
014572179502100606
Amirian, H., Solimani, S., Maleki, F., Ghasemi,
S, R., R., S., & Gilan N, R. (2017). A
Study on Health-Related Quality of
Life, Depression, and Associated
Factors Among Parents of Children
with Autism in Kermanshah, Iran.
Iranian Journal of Psychiatry and
Behavioral Sciences, 11(2). https://
doi.org/10.5812/ijpbs.7832.
Cherry D. B. (1989). Stress and coping in
families with ill or disabled children:
application of a model to pediatric
therapy. Physical & occupational
therapy in pediatrics, 9(2), 11–32. Delamater, A. M., Jacobson, A. M., Anderson,
B., Cox, D., Fisher, L., Lustman, P.,
Rubin, R., Wysocki, T., & Psychosocial
Therapies Working Group (2001).
Psychosocial therapies in diabetes:
report of the Psychosocial Therapies
Working Group. Diabetes care, 24(7),
1286–1292. https://doi.org/10.2337/
diacare.24.7.1286
Faulkner, M. S., & Clark, F. S. (1998). Quality
of life for parents of children and
adolescents with type 1 diabetes. The
Diabetes educator, 24(6), 721–727.
h t t p s : / / d o i . o r g / 1 0 . 1 1 77 /
014572179802400607
Feeley, C. A., Turner-Henson, A., Christian,
B. J., Avis, K. T., Heaton, K., Lozano,
D., & Su, X. (2014). Sleep Quality,
Stress, Caregiver Burden, and Quality
Of Life in Maternal Caregivers of
Young
Children
with
Bronchopulmonary Dysplasia. Journal
of Pediatric Nursing, 29(1), 29–38.
h t t p s : / / d o i . o r g / 1 0 . 1 0 16 /
j.pedn.2013.08.001
Herbert, L. J., Clary, L., Owen, V., Monaghan,
M., Alvarez, V., & Streisand, R. (2014).
Relations among school/daycare
functioning, fear of hypoglycaemia
and quality of life in parents of young
children with type 1 diabetes. Journal
of Clinical Nursing, 24(10), 1199
1209. https://doi.org/10.1111/
jocn.12658
Hilliard, M. E., Herzer, M., Dolan, L. M., &
Hood, K. K. (2011). Psychological
screening in adolescents with type 1
diabetes predicts outcomes one year
later. Diabetes Research and Clinical
Practice, 94(1), 39–44. https://
d o i . o r g / 1 0 . 1 0 1 6 /
j.diabres.2011.05.027
Hirose, M., Beverly, E. A., & Weinger, K.
(2012). Quality of Life and
Technology: Impact on Children and
Families With Diabetes. Current
Diabetes Reports, 12(6), 711–720.
https://doi.org/10.1007/s11892-012
0313-4
Hsieh, R. L., Huang, H. Y., Lin, M. I., Wu, C.
W., & Lee, W. C. (2009). Quality of
life, health satisfaction and family
impact on caregivers of children with
developmental delays. Child: care,
health and development, 35(2), 243
249. https://doi.org/10.1111/j.1365
2214.2008.00927.x
Janse, A. J., Sinnema, G., Uiterwaal, C. S. P.
M., Kimpen, J. L. L., & Gemke, K. J. B.
J. (2005). Quality of life in chronic
illness: Perceptions of parents and
paediatricians. Archives of Disease in
Childhood, 90(5), 486–491. https://
doi.org/10.1136/adc.2004.051722
Kahanovitz, L., Sluss, P. M., & Russell, S. J.
(2017). Type 1 Diabetes – A Clinical
Perspective. Point of care, 16(1), 37
40. https://doi.org/10.10 97/
POC.0000000000000125
Keklik, D., Bayat, M., & Baºdaº, O. (2020).
Care burden and quality of life in
mothers of children with type 1
diabetes mellitus. International Journal
of Diabetes in Developing Countries.
https://doi.org/10.1007/s13410-020
00799-3
Keklik, D., Bayat, M., & Baºdaº, O. (2020).
Care burden and quality of life in
mothers of children with type 1
diabetes mellitus. International Journal
of Diabetes in Developing Countries.
https://doi.org/10.1007/s13410-020
00799-3
Koc, G., Bek, S., Vurucu, S., Gokcil, Z., &
Odabasi, Z. (2019). Maternal and
paternal quality of life in children with
epilepsy: Who is affected more?
Epilepsy & Behavior, 92(1), 184–190.
h t t p s : / / d o i . o r / 1 0 . 1 0 1 6 /
j.yebeh.2018.12.029 Mahani, M. K., Rostami, H. R., & Nejad, S. J.
(2013). Investigation of Quality-of-Life
Determinants Among Mothers of
Children with Pervasive Developmental
Disorders in Iran. Hong Kong Journal
of Occupational Therapy, 23(1), 14
19.
https://doi.org/10.1016/
j.hkjot.2013.03.002
Mittayi.(2017).Mittayi programme under
Kerala social security mission.
Retrieved
from
https://
www.mittayi.org/home/services
Ozyazýcýoglu, N., Avdal, E. U., & Saglam, H.
(2017). A determination of the quality
of life of children and adolescents with
type 1 diabetes and their parents.
International Journal of Nursing
Sciences, 4(2), 94–98. doi: 10.1016/
j.ijnss.2017.01.008
Pierce, J. S., Kozikowski, C., Lee, J. M., &
Wysocki, T. (2017). Type 1 diabetes
in very young children: a model of
parent and child influences on
management and outcomes. Pediatric
diabetes, 18(1), 17–25. https://
doi.org/10.1111/pedi.12351
Sathyananda, R., B, & Manjunath., U. (2017).
Assessment of quality of life among
the health workers of primary health
centers managed by a nongovernment
organization in Karnataka, India: A
case study. International Journal of
Health Allied Science,6(4). https://
www.ijhas.in/text.asp?2017/6/4/240/
220518
Siboni, F, S., A., Z., Atashi, V., Alipour, M., &
Khatooni, M. (2019). Quality of Life in
Different Chronic Diseases and Its
Related Factors. International journal
of preventive medicine, 10. https://
doi.org/10 .4103/ijpvm.IJPVM_429_17
Spezia Faulkner, M., & Clark, F. S. (1998).
Quality of Life for Parents of Children
and Adolescents with Type 1 Diabetes.
The Diabetes Educator, 24(6), 721
727. https://doi.org/10.1177/
014572179802400607
Spore,E. (2012). The Quality of Life of Primary
Caregivers of Children with Chronic
Conditions [Doctoral dissertation,
University of Illinois]. University
Library. https://indigo.uic.edu/
articles/thesis/The Quality of Life
ofCaregivers of Children with Chronic
Conditions/10809086/1
The World Health Organization quality of life
assessment (WHOQOL): Position
paper from the World Health
Organization. (1995). Social Science
& Medicine, 41(10), 1403–1409.
https://doi.org/10.1016/0277
9536(95)00112-k
Thorsteinsson, E. B., Loi, N. M., & Rayner, K.
(2017). Self-efficacy, relationship
satisfaction, and social support: the
quality of life of maternal caregivers
of children with type 1 diabetes.
PeerJ,23(5). https://doi.org/10.7717/
peerj.3961
Toledano-Toledano, F., Moral de la Rubia, J.,
Nabors, L. A., Domínguez-Guedea, M.
T., Salinas Escudero, G., Rocha Pérez,
E., Luna, D., et al. (2020). Predictors
of Quality of Life among Parents of
Children with Chronic Diseases: A
Cross-Sectional Study. Healthcare,
8(4). Retrieved from http://
d x . d o i . o r g / 1 0 . 3 3 9 0 /
healthcare8040456
Uhm, J. Y., & Kim, M. S. (2020). Predicting
Quality of Life among Mothers in an
Online Health Community for Children
with Type 1 Diabetes. Children (Basel,
Switzerland), 7(11). https://doi.org/
10.3390/children7110235.
Vehik, K., Hamman, R. F., Lezotte, D., Norris,
J. M., Klingensmith, G., Bloch, C.,
Rewers, M., & Dabelea, D. (2007).
Increasing incidence of type 1 diabetes
in 0- to 17-year-old Colorado youth. Diabetes care, 30(3), 503–509. https:/
/doi.org/10.2337/dc06-1837
Wiedebusch, S., Pollmann, H., Siegmund, B.,
& Muthny, F. A. (2008). Quality of life,
psychosocial strains, and coping in
parents of children with haemophilia.
Haemophilia, 14(5), 1014–1022.
https://doi.org/10.1111/j.1365
2516.2008. 01803.x
Witt, W. P., Litzelman, K., Wisk, L. E., Spear,
H. A., Catrine, K., Levin, N., & Gottlieb,
C. A. (2010). Stress-mediated quality
of life outcomes in parents of
childhood cancer and brain tumor
survivors: a case-control study.
Quality of life research: an
international journal of quality-of-life
aspects of treatment, care and
rehabilitation,
World Health Organisation Global Report on
Diabetes. (2016). Global Report on
Diabetes. Retrieved from https://
apps.who.int/iris/bitstream/handle/
10665/204871
Yamada, A., Kato, M., Suzuki, M., Suzuki, M.,
Watanabe, N., Akechi, T., & Furukawa,
T. A. (2012). Quality of life of parents
raising children with pervasive
developmental disorders. BMC
Psychiatry, 12(1). https://doi.org/
10.1186/1471-244x-12-119
Zhan L. (1992). Quality of life: conceptual and
measurement issues. Journal of
Advanced Nursing, 17(7), 795–800.
https://doi.org/10.1111/j.1365
2648.1992.tb02000.x
Zhang, Y., Wei, M., Shen, N., & Zhang, Y.
(2015). Identifying factors related to
family management during the coping
process of families with childhood
chronic conditions: a multi-site study.
Journal of Pediatric Nursing, 30(1),
160–173. https://doi.org/10.1016/
j.pedn.2014.10.002
Conflict of interest: None
Role of funding source: None


