Indian Journal of Health Social Work
(UGC Care List Journal)
A Case of Person with Premature Ejaculation: Psychiatric Social Work Intervention
Debashree Biswas1, Nilesh Maruti Gujar2 & Arif Ali3
1M.Phil Trainee & 3Associate Professor, Department of Psychiatric Social Work, LGB Regional Institute of Mental Health, Tezpur (784001), Assam, India. 2Associate Professor, Department of Psychiatric Social Work, Centre of Excellence for Mental Health, INHS, Asvini, Colaba, Mumbai.
Correspondence: Nilesh Maruti Gujar, e-mail id: psynilesh@gmail.com
ABSTRACT
Background: Premature ejaculation (PME) is observed by an increase in erectile dysfunction with age across the lifespan of adults. PME is common but less understood sexual dysfunction among males. PME has an impact on an individual’s psychological wellbeing and interpersonal relationship with a partner. Aim: The aim of the study the impact of PME on an individual’s psychological wellbeing and to provide psychosocial intervention to cope with PME. Materials and Methods: The present case study was a single subject case study. A person diagnosed with premature ejaculation was selected purposefully from the out-patient department of LGBRIMH, Tezpur. The case was informed about the purpose and benefits of the assessment and intervention. Informed consent was taken before assessment and intervention. Psychiatric Social Work assessment for pre and post-baseline data was done using clinical and social history proforma.WHO-5 Wellbeing index, Arizona sexual experience scale, Perceived Stress Scale, Index of Premature Ejaculation. Psychiatric social work intervention was provided in order o help the client with his problems related to PME. Results: Pre-intervention results found unsatisfied sexual functions, high perceived stress, dysfunction in sexual experiences, and the average quality of life. The post-intervention results showed changes like improvement in perceived stress, quality of life, and sexual satisfaction, control over ejaculation and improved distress. Conclusion: Psychiatric social work interventions can help the client to deal with PME in effective ways.
INTRODUCTION
Sexual dysfunctions in males, premature ejaculation is one of the most prevalent sexual dysfunction among males. Erectile dysfunction is incidences are more often than other common sexual dysfunctions (Frank et al., 1978). A sexual dysfunction is found mostly in the male who experiences premature ejaculation often within a short period before or during vaginal penetration. This experiences of inability to delay ejaculation or vaginal penetrations often lead to negative personal consequences like distress, bother,
frustration and avoidance of sexual intimacy with a partner (American Psychiatric Association, 2013; McMahon et al., 2008). There are different causal factors involved like genetic, somatic, neurological and biological factors. Interpersonal issues, performance anxiety, distorted thoughts as psychological factors (Althof et al., 2014). It may cause mental distress, anxiety, embarrassment, and depression; however, most men with PME do not seek help (Porst et al., 2007). PME severely impairs sexual relationships (McCabe, 1997) and quality of life (Rowland & Slob, 1997). The present case study assessed the psychosocial impact of premature ejaculation and provides psychosocial
intervention to the client. The objectives were to assess sexual experiences, perceived stress and premature ejaculation, and to provide psychosocial intervention.
MATERIALS AND METHOD
We used a single case study design and compared pre and post-intervention data (A-B-A model). The aim was to establish a cause and effect relationship between the variables of the study and/ or to evaluate the effectiveness of the introduced program to the subject (Goodwin, 2008). The client was explained about the purpose and need for intervention after which consent was obtained before the assessment and intervention. Arizona Sexual Experiences Scale (ASEX; McGahuey et al., 1997), Perceived Stress Scale (PSS; Cohen et al., 1983), Index of Premature Ejaculation (IPE; Althof et al., 2006) and World Health Organization-5 Wellbeing Index (WHO-5 wellbeing index; World Health Organization, 1998) measurement were used in the present study.
CASE INTRODUCTION
The index client was 35 years old male Hindu, unmarried, and hailing from a middle socio- economic background of Nagar Bera Pukhuri Para, Kamrup District of Assam. The information was gathered from the client himself, his girlfriend, and the client case record file. The information gathered was reliable and adequate. The case was referred for adequate psychosocial assessment and intervention.
Brief clinical history
The index client was brought to LGBRIMH, Tezpur for treatment with the illness of gradual onset, continuous course and deteriorating progress with the chief complaints of anger outburst, decrease sleep, nightfall (ejaculation of semen’s while sleeping ), pre-ejaculation, and decreased sexual energy for last 14 months .During the detailed interview, client expressed details about his experiences with premature ejaculation. The client
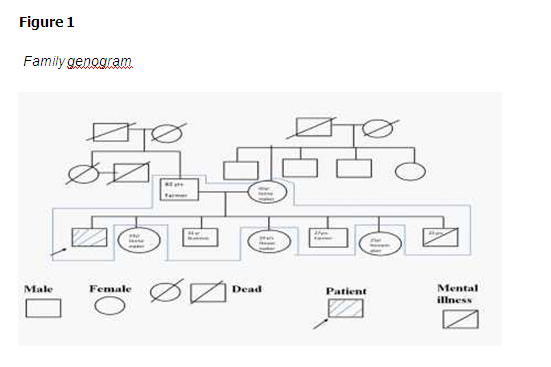
Family dynamics
The family consists of subsystems like parental, siblings, patent child sub-systems. The different subsystems aligned well with each other, boundary are open and clear, communication pattern is healthy, they have cordial interactions, healthy emotional attachment and support each other during a time of crisis.
RESULTS
Perceived stress improved from high stress (28) to moderate stress (19) in post-assessment. Overall sexual experiences were found dysfunctional at pre (20) and post (18) tests. The post-intervention changes found changes in wellbeing from average (14; 56%) quality of life to good (21; 84%) quality of life (table 1). Figure 2 represents that psychiatric social work intervention showed changes in client’ s experiences of premature ejaculation including the domain of sexual satisfaction improved from 26.4 to 51.3, control domain from 21.5 to normal 39.6 and distress reduced from 31.6 to 60.1.


Psychiatric social work intervention
sychiatric social work intervention was provided in a two way in which face to face sessions occurred in OPD setting and telephonic sessions. The intervention was targeted towards his experiences related to premature ejaculation. A total of 18 sessions (10 face to face and 8 telephonic), one session per week. The intervention was carried out over five months from February 2020 to June 2020.
Rapport building and therapeutic alliance
The rapport was established with empathic listening and understanding the problems that the client has been facing and assuring confidentiality. The therapist in this session explained to the client the importance of non-pharmacological treatment and how it would help him to cope with the illness.
Psychoeducation
The client was psycho educated about the nature of the illness, causes, and the various treatment options. In sexual dysfunction psychoeducation interventions focuses on behaviour repertoire associated with individuals or couples sexual script (Gagnon et al., 1982). We assessed and discussed myths and misconceptions regarding sexual activity. The poor knowledge and understanding were clarified by imparting factual information about PME.
Supportive intervention
Patient’s with PME often represents distress regarding their condition (Melnik et al., 2011; Shabsigh, 2006). Concerns like distress, bother, frustration avoidance due to PME are heard and the client was supported to ventilate these concerns. The education regarding PME was given and the client was reassured how the treatment can help him to overcome his condition.
Start-stop technique
The start-stop technique and Squeeze technique was discussed with the client to gain more control over ejaculation (Semans, 1956). Both the partners were instructed to extend co-operation to one another during the intercourse.
Cognitive-behavioral therapy
Cognitive behavior therapy is valuable in treating a range of emotional disorders (Beck, 2005). The goal was to increase understanding about his problems, improve coping, reduction in distress associated with premature ejaculation. The model emphasizes the deceptively simple notion that the way a person makes a sense of an event determines how the person feels and behaves. Cognitive behavior techniques focus on dysfunctional beliefs which maintain negative thoughts about sexual dysfunctions (McCabe et al., 2010; Althof, 2010). Using restructuring techniques these thoughts were addressed through the ABCD method. Talking back to his thoughts using the A- B-C-D method (A- Activating event, B – belief or thought he has, C- consequence and D-dispute or talk back to the thought) related to PME. The client was encouraged on ways to increase healthy thinking.
Relaxation technique
Physiological relaxation helps patients with PME to have better control over their bodies. Relaxation training benefits in satisfactory sexual functions. The relaxation training can be given in the form of breathing exercise, body awareness and muscle relaxation to improve bodily tensions and enhance physical sensations (Metz et al., 2000). The session was conducted to teach the client some of the relaxation techniques which would help him to reduce his stress and anxiety. We taught him deep breathing exercises and the same was given as homework tasks to practice. Another technique was taught which was imagery thinking of some of the favorite places and going through each of the senses and imagining the experiences from the relaxing place. Muscle relaxation technique was also suggested to the client.
Outcome of interventions
The intervention could help the client to clear information on PME, the knowledge over illness and its treatment modalities were well imparted. The intervention helped the client to reduce distress, frustration and anxious thoughts of the client. The client was found to be feeling relief, good emotional state.
DISCUSSION
The psychiatric social work intervention was found to be effective in dealing with problems associated with PME. Waldinger (2008) explained that the life lone PME requires medication treatment but psychoeducation, reassurance and other non- pharmacological interventions are the first choices of treatment for persons with pre-mature ejaculation. Our study found changes in the client’s sexual experiences like improvement in distress and control. Sex therapy can be part of mainstream treatment while dealing with persons with premature ejaculation/ sexual dysfunction (Hogan, 1978). The pause and squeeze techniques (Van Lankveld et al., 2009; Masters & Johnson, 1970; Semans, 1956) are widely used and effective in sexual dysfunction and premature ejaculation whereas there are some other adjourn to it was client’s attention on his physical sensations before orgasm(Kaplan ,1974) and operant shaping and time out for reinforcement (Tanner, 1973).
In the future longitudinal studies can be done to observe the long term effects of the treatment. The intervention module needs to be modified as per the socio-cultural background of the cases. The psychiatric social work professionals can promptly select this treatment approach as it does help along with pharmacological interventions rather than primary interventions in most cases.
CONCLUSION
Psychiatric social work interventions for the treatment of pre-ejaculation cover a diverse array of treatment interventions. Psychosocial intervention can be effective in addressing the psychosocial issues associated with premature ejaculation.
REFERENCES
Althof, S. (2010). Development and validation of a new questionnaire for the assessment of subjective physical performance in adult patients with haemophilia – the HEP-Test-Q. Haemophilia.
Althof, S. E. (2010). What’s new in sex therapy (CME). The Journal of Sexual Medicine, 7(1), 5-13.
Althof, S. E., McMahon, C. G., Waldinger, M. D., Serefoglu, E. C., Shindel, A. W., Adaikan, P. G., … & Torres, L. O. (2014). An update of the International Society of Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation (PE). The Journal of Sexual Medicine, 11(6), 1392-1422.
Althof, S., Rosen, R., Symonds, T., Mundayat, R., May, K., & Abraham, L. (2006). Development and validation of a new questionnaire to assess sexual satisfaction, control, and distress associated with premature ejaculation. The Journal of Sexual Medicine, 3(3), 465-475.
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). 5th ed. Arlington, VA: American Psychiatric Association. http://www.psychiatry.org/ dsm5.
Bech, P., Gudex, C., & Johansen, K. S. (1996). The WHO (Ten) well-being index: validation in diabetes. Psychotherapy and Psychosomatics, 65(4), 183-190.
Beck, A. T. (2005). The current state of cognitive therapy: a 40-year retrospective. Archives of General Psychiatry, 62(9), 953-959.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385-396.
Frank, E., Anderson, C., & Rubinstein, D. (1978). Frequency of sexual dysfunction in “normal” couples. New England Journal of Medicine, 299(3), 111-115.
Gagnon, J. H., Rosen, R. C., & Leiblum, S. R. (1982). Cognitive and social aspects of sexual dysfunction: Sexual scripts in sex therapy. Journal of Sex & Marital Therapy, 8(1), 44-56.
Goodwin, M. S., Velicer, W. F., & Intille, S. S. (2008). Telemetric monitoring in the behavior sciences. Behavior Research Methods, 40(1), 328-341.
Hogan, D. R. (1978). The effectiveness of sex therapy: A review of the literature. Handbook of Sex Therapy, 57- 84.
Kaplan, H. S. The new sex therapy. New York: Brunner/Mazel, 1974. Masters, W. H., & Johnson, V. E. (1970). Human sexual inadequacy. Little Brown. Co.., Boston.
McCabe, M. P. (1997). Intimacy and quality of life among sexually dysfunctional men and women. Journal of Sex & Marital Therapy, 23(4), 276-290.
McCabe, M., Althof, S. E., Assalian, P., Chevret- Measson, M., Leiblum, S. R., Simonelli, C., & Wylie, K. (2010). Psychological and interpersonal dimensions of sexual function and dysfunction. The Journal of Sexual Medicine, 7(1), 327-336.
McGahuey, C. A., Gelenberg, A. J., Laukes, C., Manber, R., McKnight, K., Moreno, F. A., & Delgado, P. L. (1997). The Arizona Sexual Experiences Scale (ASEX): Validity and reliability, 150th Annual Meeting of the American Psychiatric Asso- ciation, San Diego, CA, NR # 184, May 19, 1997.
McMahon, C. G., Althof, S. E., Waldinger, M. D., Porst, H., Dean, J., Sharlip, I. D., … & Segraves, R. (2008). An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. The Journal of Sexual Medicine, 5(7), 1590-1606.
Melnik, T., Althof, S., Atallah, Á. N., dos Santos Puga, M. E., Glina, S., & Riera, R. (2011). Psychosocial interventions for premature ejaculation. Cochrane Database of Systematic Reviews, (8).
Metz, M. E., Pryor, J. L. (2000). Premature ejaculation. A psychophysiological approach for assessment and management. Journal of Sex & Marital Therapy, 26 (4), 293–320.
Porst, H., Montorsi, F., Rosen, R. C., Gaynor, L., Grupe, S., & Alexander, J. (2007). The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: prevalence, comorbidities, and professional help- seeking. European Urology, 51(3), 816-824.
Rowland, D. L., & Slob, A. K. (1997). Premature ejaculation: psychophysiological considerations in theory, research, and treatment. Annual Review of Sex Research, 8(1), 224-253.
Semans, J. (1956). Premature ejaculation: a new approach. Southern Medical Journal, 49(4), 353-357.
Shabsigh, R. (2006). Diagnosing premature ejaculation: a review. The Journal of Sexual Medicine, 3, 318-323.
Tanner, B. A. (1973). Two case reports on the modification of the ejaculatory response with the squeeze technique. Psychotherapy: Theory, Research & Practice, 10(4), 297-300.
Topp, C. W., Østergaard, S. D., Søndergaard, S., & Bech, P. (2015). The WHO-5 Well-Being Index: a systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167-176.
Van Lankveld, J. J., Leusink, P., Van Diest, S., Gijs, L., & Slob, A. K. (2009). Internet-based brief sex therapy for heterosexual men with sexual dysfunctions: a randomized controlled pilot trial. The Journal of Sexual Medicine, 6(8), 2224-2236.
Waldinger, M. D. (2008). Recent advances in the classification, neurobiology and treatment of premature ejaculation. Sexual Dysfunction, 29, 50-69.
World Health Organization, Regional Office for Europe, 1998. Use of well-being measures in primary health care – the DepCare project health for all. Target 12. E60246. Geneva: WHO.
Conflict of interest: None
Role of funding source: None


