Indian Journal of Health Social Work
Barriers, Cultural Variance and Pathways to Psychiatric Care: A Systemic Review
Mamata Swain1, Indrajeet Banerjee2, Arif Ali3
1PhD Scholar, Department of PSW, LGBRIMH,Tezpur, 2Assistant Professor, Department of PSW, LGBRIMH, Tezpur, 3Associate Professor, Department of PSW, LGBRIMH, Tezpur.
Correspondence: Mamata Swain, e-mail id: swain.mamta805@gmail.comABSTRACT
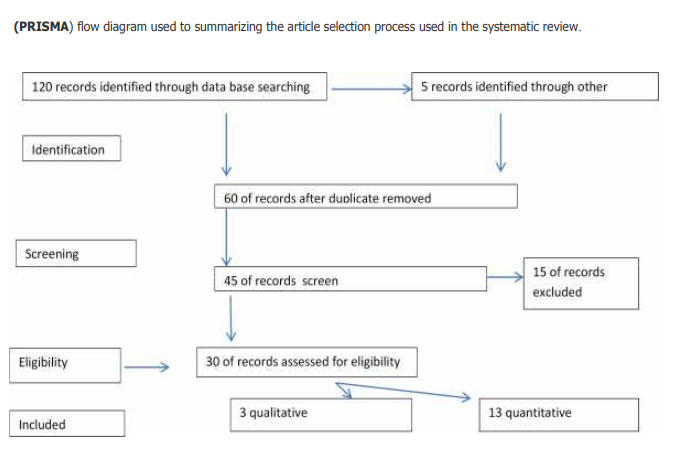
Background: Psychiatric illness is mostly chronic in nature and due to delay in treatment process the level of functioning is highly impaired along with it have a direct impact on individual quality of life. According to the National Report of NMHS reveals that nearly 83% people of India are need of active interventions for one or more mental health issues. Most of the identified had not sought for treatment or not able to access appropriate care despite seeking. The treatment gaps are huge in both rural and urban settings with direct or indirect influence of multiple factors. Materials and Methods: Systematically review of the literature was carried out to find out the barriers and cultural differences in pathways to psychiatric care among the patients with first episode psychosis. Studies were identified through searches of various electronic database (MEDLINE, PsycINFO, SCIENCEDIRECT, PubMED, Health STAR and CINAHIL) supplemented by backward and forward mapping and hand searching and citation tracing was carried out. We included studies on the pathways to psychiatric care of individuals aged 18-60years, both genders, written in English language and were published between 2010 to 2020.Two reviewers independently screened articles and extracted data. Results and Conclusion: The most common type of barriers mostly identified in the literature is Mental Health literacy and cost of the treatment followed by Structural barriers and negative experiences with the professionals played a key role in not approaching MHS. The most common reasons for drop-out from professional services included perceived ineffectiveness of treatment and negative experiences with treatment providers.
INTRODUCTION
India is a country with cultural diversity with differing rates of ethnic groups and mental health problems, particularly psychosis, which is reflection on their diverse cultural and socio- economic background. It is essential that all culturally different groups have access to mental health services and adequate treatment. According to the National Report of NMHS reveals that nearly 83% people of India are need of active interventions for one or more mental health issues. Most of the identified had not sought for treatment or not able to access appropriate care despite seeking. The treatment gaps are huge in both rural and urban settings with direct or indirect influence of multiple factors. Cultural difference has the potential to influence the nature and direction of pathways to care .For the present study cultural difference described the social group of person belongs to based on factors such as language, religion and belief system. An individual’s cultural background influences decisions about whether and how to seek help, as well as the array of services and supports that are available to the persons throughout the help-seeking process.Other factors known to covary with cultural difference group, such as poverty and discrimination may also influence the pathways to care process and economic condition and language barriers may delay access to care.
AIM
The aim of the present study was to systematically review the literature on barriers and cultural differences in pathways to care among the patients with first-episode psychosis to determine the factors responsible in delay help seeking behaviour. Because the pathways to care are affected by the availability and accessibility of services within a given health system, and there are differences in service provision in developed and developing countries, our review focused on specific questions (a) why? How to reach and don’t reach to psychiatric hospital (b) what are the different kind of barriers which restricted the individual or delay the process of seeking the adequate services.
MATERIALS AND METHODS
We included published papers that compared access to, or use of mental health services in India. We included studies carried out on adult population with first episode psychosis and excluded children and substance misuse. The following bibliographic database were searched, (MEDLINE, PsycINFO, SCIENCEDIRECT, PubMED, Health STAR and CINAHIL) with additional searches were carried out through google scholar with search terms were followed as psychosis, mental illness, culture, and barriers supplemented by backward and forward mapping and hand searching and citation tracing was carried out. We included studies on the pathways to psychiatric care of individuals aged 18-60years, both genders, barriers, cultural difference, written in English language and were published between 2010 to 2020. General and conceptual articles, letters to the editor, case studies, poster presentation were excluded in the review process.
RESULTS & DISCUSSION
Based on the content analysis technique six themes and 21 subthemes were identified which describe the barriers in pathways to care among the PWMI. The most common type of barriers mostly identified in the literature is Mental Health literacy and cost of the treatment followed by Structural barriers and negative experiences with the professionals played a key role in not approaching MHS. The most common reasons for drop-out from professional services included perceived ineffectiveness of treatment and negative experiences with treatment providers (Andrade et al ., 2014). Negative experiences with healthcare providers, confidentiality, stigma, distance and loss of hope are reported in few studies (Mathias et al., 2019). Majority of studies reported that primarily faith healers are the first choice of pathways to care. Urban people are late to Mental health consultation in compared to rural sample and distance was one of the major factor for discontinuation of services or not seeking help from the MHP.(Jain et al., 2012)
In a nutshell, studies focusing mainly on relationship or correlates of different factors related to delayed in choosing appropriate pathway options. Though, few studies examined certain correlates of treatment delay, most of them have identified stigma, poor awareness about illness and cost of service as factors of concern. The influence of other factors is unclear and an overall picture is not portrayed. So far studies have exclusively carried out on sequence of pathways along with duration of untreated illness. However, there were insufficient studies examining the role of culture in Indian context. There is a need for large sample studies, particularly on samples of non-treatment seekers from different socio-cultural backgrounds which systematically examine the role of various barriers to pathways and to find out any differences in factors related to selection of pathways between different psychiatric disorders. Demand-side barriers also require attention to managing supply-side barriers for reducing the treatment gap for mental health problems in the Indian context.
CONCLUSION
Studies across the sections reveal that pathways is a complex process and influenced by multiple interacting factors. It repeatedly emerges in the studies that mere knowledge about the illness and availability of professional services is insufficient to minimize the delays in professional help-seeking behaviour. Moreover, the review suggests that the pathways often involves a shared collective decision making process or the selection of pathways is often influenced by the recommendations of one’s social networks (Prabhu et al., 2015). It seems to be a reflection of a predominantly collective orientation that characterizes the Indian culture and places a higher value on interdependence and social harmony (Chadda et al., 2013). These patterns are in line with the previous observations that cultural differences and barriers in selection of pathways exist.
IMPLICATION
However there is a need to plan for an effective psych educational model or community level awareness programme based on explanatory model of illness without challenging individual indigenous belief system and focused on the coping method. Involvement of different level of stakeholders in the process of early identification through task-shifting approach.
REFERENCES
Behari M, Gupta DK, Singh V, Verma KK, Sengupta SN, Sidana R, et al (2013) . Help seeking behavior and pathways to care among patients seeking care at a community mental health clinic and psychiatry outpatient department of a medical college: A study from North Rajasthan. J Ment Health Hum Behav ,18,18-33.
Gupta, D.K., Sidana, R., Behari, M., Verma, K.K.,Bhadoriya, M.S.(2018). Help-seeking behavior and pathways to care among patients seeking treatment at a private psychiatric hospital in North India. Journal of Ment Health Hum Behav , 23(1),63-66.
Gupta, S.K. (2012). Web model of pathways to psychiatric care for Indian setting. International Journal of Health and Allied Sciences,1(4), 293-296
Khemani, M.C., Premaranjan, K.C.,Menon, V.,Olikal,J.J et al., (2020). Pathways to care among patients with severe mental disorders attending a tertiary health care facilities in Puducherry South India. Indian Journal of Social Psychiatry .62(6),664- 669.
Korem, A., Bogaraju, A., L.V.R Usha (2017) Help- seeking behaviors in the relatives of mentally Ill persons at a Tertiary Care Hospital. Indian Journal of Social Psychiatry,33(3), 250-255.
Lamichhane, N., Thapa, D.K., Timsina, R.R., Sharma, R., Vaidya, L., Subedi, A. (2019) Pathway to Care of Psychiatric Services in Gandaki Medical College Teaching Hospital in Western Nepal. Journal of Gandaki Medical College-Nepal.12(2), 80- 85.
MacDonald, K., Fainman-Adelman, N., Anderson, K.K. et al. (2018). Pathways to mental health services for young people: a systematic review. Soc Psychiatry Psychiatr Epidemiol 53, 1005–1038
Mishra, N., Nagpal, S. S., Chadda, R. K., & Sood, M. (2011). Help-seeking behavior of patients with mental health problems visiting a tertiary care center in north India. Indian journal of psychiatry , 53(3), 234–238.
Mutalik, N.R., Dewani, K., and Shriniwas, B.C. (2017). Pathways to psychiatric care: -A hospital-based study. Journal of Medical Science and Clinical Research, 5 (4).
Naqvi, H.A., Hussain, S., Zaman, M., Islam, M. (2009) Pathways to Care: Duration of Untreated Psychosis from Karachi, Pakistan. PLOS ONE 4(10)
Reddy, K.S., Thirthalli, J., Channaveerachari, N., Reddy, K., Ramareddy, R., Rawat, V., et al. (2014). Factors influencing access to psychiatric treatment in persons with schizophrenia: A qualitative study in a rural community. Indian Journal Psychiatry 56(1):54–60.
Trivedi, J. K., & Jilani, A. Q. (2011). Pathway of psychiatric care. Indian journal of psychiatry, 53(2), 97–98.
Conflict of interest: None
Role of funding source: None


