Indian Journal of Health Social Work
(UGC Care List Journal)
QUALITY OF LIFE AMONG THE FAMILIES OF ALCOHOL ADDICTION TRIBES STAYING IN SOUTH KARNATAKA
Jyothi H.P1 , Kannappa V Shetty2 , Amritha3 , Suparna.S4 , Sachetha GM51Associate Professor, Department of Social Work, Mysore University, Mysore. 2Assistant Professor, School of Social Work, Indira Gandhi National Open University (IGNOU), New Delhi,.3Ph.D scholar, SOSW, IGNOU, New Delhi. 4Counselling Psychologist, Amrita Vishwa Vidyapeetham Bengaluru . 5Ph.D scholar, SOSW, IGNOU, New Delhi
Correspondence: : Kannappa V Shetty, e-mail: vksettymsw@gmail.com
ABSTRACT
Background: The quality of life among tribal members who care for people with alcohol addiction in their community sheds light on the unique challenges they encounter and potential sources of assistance. Caregivers in tribes impacted by dependency on alcohol often experience an array of obstacles that adversely affect their standard of life. The intergenerational trauma, cultural stigmas associated with alcoholism, and limited access to resources exacerbate the problems faced by these caregivers. Despite these challenges, caregivers show resiliency and dedication to their work, trying to assist and care for their loved ones in the face of hardship. Methods & Materials: Aim: The study aims to understand the quality of life among the caregivers of alcoholaddicted individuals in the tribal community of Karnataka. A descriptive research design, with a sample size of 150 Soliga tribal adults was conducted in the southern Karnataka state. A semistructured interview schedule along with the Quality-of-Life Scale (WHOQOL) was used. Results: 45% of the tribal patients with ADS were illiterates. 87% of the caregivers were female, mostly spouses, 98% of the respondents had a Family History of ADS. The respondents were spending Rs 3776 per month on alcohol. The study show that the quality of life of caregivers, particularly elderly caregivers, is adversely impacted in the areas of physical, psychological, and social interactions, as well as the environment. Conclusions: Overall, the burden for caregivers of patients with ADS in the Mysore tribal region has a significant impact on their quality of life.Keywords:ADS, Quality of life, Tribes, Caregivers/family, Mental Health
INTRODUCTION
According to the UN, it is estimated that there are more than 476 million indigenous population spread across 90 countries worldwide(Short & Lennox, 2013).These individuals possess distinctive social, cultural, economic and political traits, languages, knowledge, systems, beliefs, resource management techniques and hold diverse development concepts based on traditional values and priorities(Newcomb, 2011). The term “indigenous people” in India has been used for a long time, but with the term “Adivasi” referring to the tribal population. According to the 2011 census, the tribal population constituted 8.6% of the country’s population, up from 8.2% in 2001(Chandramouli & General, 2011).The tribal population in India is the poorest and most vulnerable, with a significant decline in poverty due to their low starting point. Rajasthan has the largest tribal population, constituting over 12% of the state’s population. In southern states, tribal’s reside in rural and forest dwellings in Kerala, Karnataka, Andhra Pradesh, and Tamil Nadu(Pradesh & Andhra, 2020; Sudarshan & Seshadri, 2022). Quality of life is an individual’s perspective on life influenced by cultural and value frameworks. It measures improvement in various aspects, with a healthy life, knowledge acquisition, and dignified resources being crucial(S. K. Chaturvedi & Muliyala, 2016). However, the quality of life of tribes is unique because they have been socially marginalized. In India, the biggest problems faced by tribal communities range from land alienation to alcoholism and underemployment(Vidyarthi, 1972). The tribal community’s well-being is at risk due to various diseases, malnutrition, mental illness, addictions, and poor health-seeking behaviour(Balgir, 2006). Alcohol abuse in developing countries like India is worse than the developed countries despite equal amounts of drinking. Chronic alcohol dependence is characterized by excessive and compulsive drinking that produces disturbances in the mental or cognitive level of functioning that interfere with social and economic levels (Saxena, 1997).Alcohol dependence is a harmful drinking pattern causing distress or impairment, characterized by intense cravings, gradual increase in consumption, and withdrawal symptoms. Individuals often organize their day to obtain, consume, and enjoy alcohol (Skinner & Allen, 1982). It causes financial strain, mental and physical discomfort, workplace and social dysfunction, mainly impacting individuals life and their relationships (Vaishnavi, Karthik, Balakrishnan, & Sathianathan, 2017a) . In 2004, a study by the Ministry of Social Justice and Empowerment in India and the United Nations Office of Drugs and Crime revealed that 21% of adult males and 5% of adult females consume alcohol (Benegal, 2005). Similarly, a studying Rajasthan revealed that 36% of males and 13% of females consume liquor and locally produced toddy, with higher usage reported in tribal communities (Sundaram, Mohan, Advani, Sharma, & Bajaj, 1984). The tribal population is significantly underrepresented in health indices, with women and children being the most vulnerable, and over 72% of tribal men over 15 use tobacco and drink alcohol(Debbarma, 2019). A 2017 survey in Arunachal Pradesh revealed that 49% of men and 28% of women in some indigenous tribal cultures regularly consume alcohol, indicating a higher prevalence of alcohol misuse and disease load (H. K. Chaturvedi, Bajpai, & Tiwari, 2019). A National Family Health survey shows that 26% of indigenous people consume alcohol, compared to 9% for non-indigenous populations. This disparity is linked to socioeconomic marginalization, mistreatment, and limited access to health information, leading to poverty, severe health issues, violence, and high morbidity among native tribal populations. The rate of alcohol abuse is greater within native tribal populations, and the resulting health issues have become more prevalent(Sadath, Uthaman, & Kumar, 2018; Subramanian, Smith, & Subramanyam, 2006). Karnataka was once part of several kingdoms, which is rich in its historic, cultural, and anthropological heritage and is home to 42,48,987 tribes of whom 50,870 belong to the primitive group (Chandramouli & General, 2011). Some of the known tribes in Karnataka are Soligas, Yeravas, Todas, and Siddhis who constitute 6.9% of the total population of Karnataka (Roy, Hegde, Bhattacharya, Upadhya, & Kholkute, 2015). This paper details the quality of life of caregivers of Soliga tribal about alcohol dependence on habitats in forest regions in the state of Karnataka.METHODS AND MATERIALS
Study design: It is a community-based cross-sectional study with a descriptive research designStudy setting: The population of the study consists of the male and female inhabitants of the Soliga tribes, who live in the forest regions of south Karnataka.
Sampling technique: A simple random sampling was used for the quantitative survey Sample Size: 150 respondents were selected for the study.
Inclusion and exclusion criteria: People of all age groups who were using alcohol were considered as the population of the study. Tribes staying in forests, who were willing to participate in the study and were able to understand the Kannada language were included. Those tribes who were unwilling to give consent were excluded from the study
Details on Tools
1. Semi-structured interview schedule for persons with ADS, and their caregivers: An interview schedule prepared for the assessment of personal and household details for both caregivers and persons with ADS, which includes personal and sociodemographic data.
2. Quality of Life: (World Health Organization Quality-of-Life Scale (WHOQOL): This scale is used to measure the quality of life of family members living with persons with ADS(Vahedi, 2010).
Statistical analysis: The data was entered and analyzed in SPSS 20. Categorical variables were summarized as percentages and quantitative variables were summarized as means with standard deviation (SD), with inter-quartile range (IQR) according to the distribution of the variables.
Ethical aspects: The participant’s anonymity was maintained and all participant information was kept confidential. Written informed consent was obtained from all participants. The current study received ethical clearance from the Institute Ethics Committee, Mysore University. Ref: IHEC-UOM No.82/Res/2022- 23. Dated: 24.11.2022.
1. Semi-structured interview schedule for persons with ADS, and their caregivers: An interview schedule prepared for the assessment of personal and household details for both caregivers and persons with ADS, which includes personal and sociodemographic data.
2. Quality of Life: (World Health Organization Quality-of-Life Scale (WHOQOL): This scale is used to measure the quality of life of family members living with persons with ADS(Vahedi, 2010).
Statistical analysis: The data was entered and analyzed in SPSS 20. Categorical variables were summarized as percentages and quantitative variables were summarized as means with standard deviation (SD), with inter-quartile range (IQR) according to the distribution of the variables.
Ethical aspects: The participant’s anonymity was maintained and all participant information was kept confidential. Written informed consent was obtained from all participants. The current study received ethical clearance from the Institute Ethics Committee, Mysore University. Ref: IHEC-UOM No.82/Res/2022- 23. Dated: 24.11.2022.
RESULTS
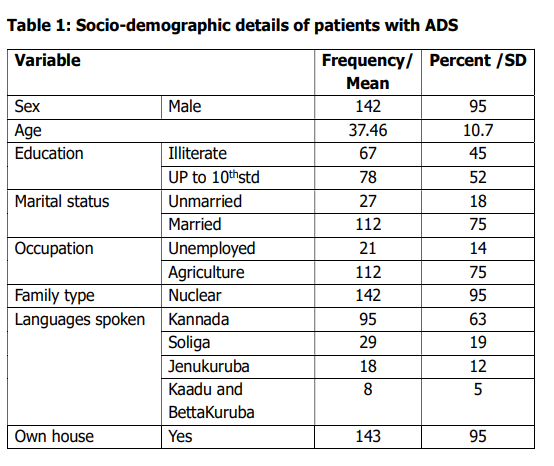
Table 1 shows the caregiver’s patients details.
The majority of patients with ADS are males,
with an average age of 37.46 (SD=10.7). They
have limited education, with 45% being
illiterate and 52% having up to the 10th
standard. Most are married, with 75%
working in agriculture and 14%is
unemployed. They mainly belong to nuclear
families residing in their own houses and
speak Kannada, followed by other languages.
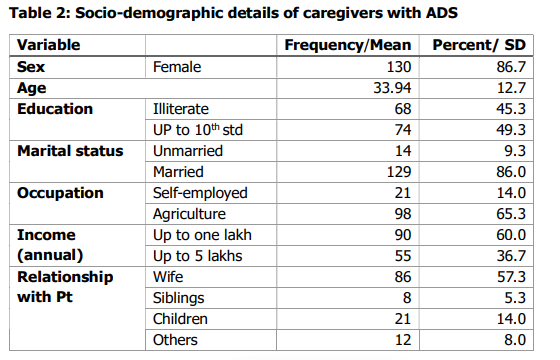
Table 2 explains the caregiver’s demographic
details. The majority of caregivers for
patients with ADS are women, with an average
age of 33.94(SD=12.7). They are
predominantly married and engaged in
agriculture or self-employment, with an
annual income of up to one lakh (60%) or up
to 5 lakhs (36.7%). Wives (57.3%) are the
primary caregivers.
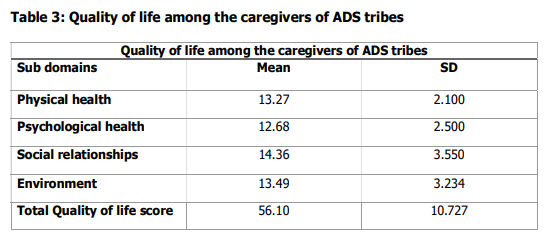
Table 3 shows caregivers’ quality of life among
ADS tribes, revealing average ratings in
physical, psychological, social, and
environmental health, resulting in an overall
score of 56.10 (SD=10.727).
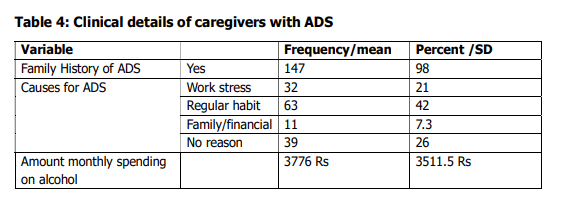
Table 4 reveals the clinical details of
caregivers with ADS. Majority have a family
history of ADS (98%), with causes attributed
to work stress (21%), regular habits (42%),
family/financial issues (7.3%), and no
specified reason (26%). The average monthly
spending for alcohol is Rs. 3776.

Table 5 shows a significant negative
correlation between patient age and the total
quality of life score (r = -0.288**), but no
significant correlation was found between
alcohol expenditure, caregiver age, and the
total quality of life score.

DISCUSSION
Alcoholism is a serious mental health condition
that is often linked to challenges(Das,
Balakrishnan, & Vasudevan, 2006). Not only
does it impact the person dealing with
addiction, but it also has a lasting impact on
caregivers and family members(Shetty,
Manikappa, Murthy, Anjanappa, & Rawat,
2022). This study is the first to explore the
quality of life of alcohol-dependent caregivers
in Karnataka tribes, revealing the profound
impact of this syndrome on their lives, and
highlighting the importance of understanding
their experiences.
This research found that 95% of caregivers’
partners with ADS were men, indicating a
higher prevalence of alcohol dependence
among tribal men(Sadath et al., 2022), with
the incidence increasing in younger
men(Mohindra, Narayana, Anushreedha, &
Haddad, 2011), as per previous studies.
The study reveals that 87% of caregivers are
women, with 98% having a family history of
ASD. Habitual drinking accounts for 42% of
alcohol dependence causes, with no specific
explanation accounting for 26%. This
highlights the inherited and early exposure to
habitual drinking, leading to the normalization
of alcoholism among abusers and caretakers.
The findings align with a previous study on
alcohol abuse among tribal men in Kerala’s
Wayanad district, which found individuals
began drinking alcohol at a young age due to
various economic, cultural, and social
factors(Sadath et al., 2019).
A large amount of research suggests a link
between abusing alcohol, unemployment, and economic strain(Vaishnavi, Karthik,
Balakrishnan, & Sathianathan, 2017b). The
study reveals that over half of the participants
work in the agricultural sector, with most
earning up to 1 lakh and 38% earning up to 5
lakhs. However, the average alcohol spending
is 3779 Rs, with significant variability. This
expenditure is not justified, as most are in
nuclear families with spouses, parents,
children, and some siblings. The WHO alcohol
impact study shows that excessive alcohol
consumption harms families by increasing
debt and reducing spending on food,
necessities, and savings(Health & Abuse,
2004).
In a study on the issues of alcohol dependence
among Kerala tribes, researchers discovered
that the majority of people were exploited by
outsiders on the wage for their work by
providing substandard quality local alcohol
instead of money and that these people spent
their earnings on alcohol
consumption(Shihab, 2020). Similarly, the
Soliga tribes in this research face the same
challenge; a significant portion of their
revenue is spent on alcohol drinking, but
there is no external exploitation of the people.
The study found no significant association
between alcohol consumption and other
variables like patient age, caregiver age, or
total quality of life (Jyani, Prinja, Ambekar,
Bahuguna, & Kumar, 2019; Mohindra, et al.,
2011; Shetty, Janardhana, Math, Marimuthu,
& Rajkumar, 2022). However, there was a
significant negative correlation between
patient age and caregiver quality of life,
suggesting that as patient’s age, caregivers’
quality of life tends to decrease. This
contradicts previous studies indicating a
correlation between alcohol consumption and
overall quality of life. This could be due to
various reasons like an increase in the
complexity of care like co-morbid issues due
to prolonged alcohol intake(Sundaram, et al.,
1984), financial strain due to medication and
hospital visits(Olickal, Saya, Selvaraj, &
Chinnakali, 2021), interpersonal
issues(Sadath, et al., 2019) lack of time for
necessary self-care can all lead to emotional
strain and burnout impacting the overall
quality of life.
Large-scale community interventions are
crucial to address the complex relationship
between cultural norms and individual coping
mechanisms, especially for young people
susceptible to unhealthy practices. By focusing
on prevention and offering alternative coping
mechanisms, we can reduce the prevalence
of alcohol dependence syndrome among
tribes. Additionally, stakeholders can develop
targeted interventions that address the wellbeing of both caregivers and ADS patients,
with a particular focus on supporting older
individuals with ADS.
Financial support: This project is funded by ICSSR, Government of India, New Delhi.
Financial support: This project is funded by ICSSR, Government of India, New Delhi.
REFERENCES
Balgir, R. (2006). Tribal health problems, disease burden and ameliorative challenges in tribal communities with special emphasis on tribes of Orissa. Paper presented at the Proceedings of National Symposium on “Tribal Health” 19th-20th October. Benegal, V. (2005). India: alcohol and public health. Addiction, 100(8), 1051-1056. Chandramouli, C., & General, R. (2011). Census of india 2011. Provisional Population Totals. New Delhi: Government of India, 409-413. Chaturvedi, H. K., Bajpai, R. C., & Tiwari, P. (2019). Association of religion and cultural tradition with alcohol use among some tribal communities of Arunachal Pradesh, India. Journal of ethnicity in substance abuse, 18(2), 296-308. Chaturvedi, S. K., & Muliyala, K. P. (2016). The meaning in quality of life (Vol. 3, pp. 47-49): Springer. Das, S. K., Balakrishnan, V., & Vasudevan, D. (2006). Alcohol: its health and social impact in India. National Medical Journal of India, 19(2), 94. Debbarma, B. (2019). Behavioural Health Risks Associated with Substance Use: Tobacco and Alcohol Consumption among Ethnic Population in Tripura. Journal of North East India Studies, 9(1). Health, W. H. O. D. o. M., & Abuse, S. (2004). Global status report on alcohol 2004: World Health Organization. Jyani, G., Prinja, S., Ambekar, A., Bahuguna, P., & Kumar, R. (2019). Health impact and economic burden of alcohol consumption in India. International Journal of Drug Policy, 69, 34-42. Mohindra, K., Narayana, D., Anushreedha, S., & Haddad, S. (2011). Alcohol use and its consequences in South India: Views from a marginalised tribal population. Drug and Alcohol Dependence, 117(1), 70-73. Newcomb, S. T. (2011). The UN declaration on the rights of indigenous peoples and the paradigm of domination. Griffith Law Review, 20(3), 578-607. Olickal, J. J., Saya, G. K., Selvaraj, R., & Chinnakali, P. (2021). Association of alcohol use with quality of life (QoL): A community based study from Puducherry, India. Clinical Epidemiology and Global Health, 10, 100697. Pradesh, T., & Andhra, T. (2020). REPORT OF COMMITTEE ON FOREST AND TRIBALS IN INDIA. Roy, S., Hegde, H. V., Bhattacharya, D., Upadhya, V., & Kholkute, S. D. (2015). Tribes in Karnataka: Status of health research. Indian Journal of Medical Research, 141(5), 673-687. Sadath, A., Jose, K., Jiji, K., Mercy, V., Ragesh, G., & Arensman, E. (2022). Prevalence and determinants of substance use among indigenous tribes in South India: Findings from a tribal household survey. Journal of Racial and Ethnic Health Disparities, 1-11. Sadath, A., Jose, K., Meethal, S. T., Mathai, J. K., Venugopal, A. P., & Xavier, N. (2019). Factors associated with alcohol misuse among indigenous tribal men in Wayanad: a qualitative study. Indian journal of psychological medicine, 41(6), 516-522. Sadath, A., Uthaman, S. P., & Kumar, T. S. (2018). Mental health in tribes: A case report. Indian Journal of Social Psychiatry, 34(2), 187-188. Saxena, S. (1997). Alcohol, Europe and the developing countries. Addiction, 92, S43-S48. Shetty, K. V., Janardhana, N., Math, S. B., Marimuthu, P., & Rajkumar, R. P. (2022). Empowering the caregivers of persons with schizophrenia–A psychosocial approach. Archives of Mental Health, 23(1), 30-34. Shetty, K. V., Manikappa, S. K., Murthy, S., Anjanappa, J., & Rawat, V. S. (2022). Expressed Emotion among Families of Individuals with Alcohol Dependence Syndrome: A Pilot Study. Annals of Indian Psychiatry, 6(4), 374-377. Shihab, H. (2020). Issues of alcoholism dependence among tribes: how Koraga tribal population of Kerala find their everyday life. International Journal of Indian Psych/logy, 8(1). Short, D., & Lennox, C. (2013). Handbook of indigenous peoples’ rights: Routledge. Skinner, H. A., & Allen, B. A. (1982). Alcohol dependence syndrome: measurement and validation. Journal of abnormal psychology, 91(3), 199. Subramanian, S., Smith, G. D., & Subramanyam, M. (2006). Indigenous health and socioeconomic status in India. PLoS Medicine, 3(10), e421. Sudarshan, H., & Seshadri, T. (2022). Health of Tribal People in Central India Tribal Development Report (pp. 85-157): Routledge India. Sundaram, K., Mohan, D., Advani, G., Sharma, H., & Bajaj, J. (1984). Alcohol abuse in a rural community in India. Part I: Epidemiological study. Drug and Alcohol Dependence, 14(1), 27-36. Vahedi, S. (2010). World Health Organization Quality-of-Life Scale (WHOQOLBREF): analyses of their item response theory properties based on the graded responses model. Iranian journal of psychiatry, 5(4), 140. Vaishnavi, R., Karthik, M. S., Balakrishnan, R., & Sathianathan, R. (2017a). Caregiver burden in alcohol dependence syndrome. Journal of addiction, 2017. Vaishnavi, R., Karthik, M. S., Balakrishnan, R., & Sathianathan, R. (2017b). Caregiver burden in alcohol dependence syndrome. Journal of addiction, 2017(1), 8934712. Vidyarthi, L. (1972). Problems and prospects of tribal development in India. Indian Anthropologist, 2(2), 80-93.
Conflict of interest: None
Role of funding source: None
Balgir, R. (2006). Tribal health problems, disease burden and ameliorative challenges in tribal communities with special emphasis on tribes of Orissa. Paper presented at the Proceedings of National Symposium on “Tribal Health” 19th-20th October. Benegal, V. (2005). India: alcohol and public health. Addiction, 100(8), 1051-1056. Chandramouli, C., & General, R. (2011). Census of india 2011. Provisional Population Totals. New Delhi: Government of India, 409-413. Chaturvedi, H. K., Bajpai, R. C., & Tiwari, P. (2019). Association of religion and cultural tradition with alcohol use among some tribal communities of Arunachal Pradesh, India. Journal of ethnicity in substance abuse, 18(2), 296-308. Chaturvedi, S. K., & Muliyala, K. P. (2016). The meaning in quality of life (Vol. 3, pp. 47-49): Springer. Das, S. K., Balakrishnan, V., & Vasudevan, D. (2006). Alcohol: its health and social impact in India. National Medical Journal of India, 19(2), 94. Debbarma, B. (2019). Behavioural Health Risks Associated with Substance Use: Tobacco and Alcohol Consumption among Ethnic Population in Tripura. Journal of North East India Studies, 9(1). Health, W. H. O. D. o. M., & Abuse, S. (2004). Global status report on alcohol 2004: World Health Organization. Jyani, G., Prinja, S., Ambekar, A., Bahuguna, P., & Kumar, R. (2019). Health impact and economic burden of alcohol consumption in India. International Journal of Drug Policy, 69, 34-42. Mohindra, K., Narayana, D., Anushreedha, S., & Haddad, S. (2011). Alcohol use and its consequences in South India: Views from a marginalised tribal population. Drug and Alcohol Dependence, 117(1), 70-73. Newcomb, S. T. (2011). The UN declaration on the rights of indigenous peoples and the paradigm of domination. Griffith Law Review, 20(3), 578-607. Olickal, J. J., Saya, G. K., Selvaraj, R., & Chinnakali, P. (2021). Association of alcohol use with quality of life (QoL): A community based study from Puducherry, India. Clinical Epidemiology and Global Health, 10, 100697. Pradesh, T., & Andhra, T. (2020). REPORT OF COMMITTEE ON FOREST AND TRIBALS IN INDIA. Roy, S., Hegde, H. V., Bhattacharya, D., Upadhya, V., & Kholkute, S. D. (2015). Tribes in Karnataka: Status of health research. Indian Journal of Medical Research, 141(5), 673-687. Sadath, A., Jose, K., Jiji, K., Mercy, V., Ragesh, G., & Arensman, E. (2022). Prevalence and determinants of substance use among indigenous tribes in South India: Findings from a tribal household survey. Journal of Racial and Ethnic Health Disparities, 1-11. Sadath, A., Jose, K., Meethal, S. T., Mathai, J. K., Venugopal, A. P., & Xavier, N. (2019). Factors associated with alcohol misuse among indigenous tribal men in Wayanad: a qualitative study. Indian journal of psychological medicine, 41(6), 516-522. Sadath, A., Uthaman, S. P., & Kumar, T. S. (2018). Mental health in tribes: A case report. Indian Journal of Social Psychiatry, 34(2), 187-188. Saxena, S. (1997). Alcohol, Europe and the developing countries. Addiction, 92, S43-S48. Shetty, K. V., Janardhana, N., Math, S. B., Marimuthu, P., & Rajkumar, R. P. (2022). Empowering the caregivers of persons with schizophrenia–A psychosocial approach. Archives of Mental Health, 23(1), 30-34. Shetty, K. V., Manikappa, S. K., Murthy, S., Anjanappa, J., & Rawat, V. S. (2022). Expressed Emotion among Families of Individuals with Alcohol Dependence Syndrome: A Pilot Study. Annals of Indian Psychiatry, 6(4), 374-377. Shihab, H. (2020). Issues of alcoholism dependence among tribes: how Koraga tribal population of Kerala find their everyday life. International Journal of Indian Psych/logy, 8(1). Short, D., & Lennox, C. (2013). Handbook of indigenous peoples’ rights: Routledge. Skinner, H. A., & Allen, B. A. (1982). Alcohol dependence syndrome: measurement and validation. Journal of abnormal psychology, 91(3), 199. Subramanian, S., Smith, G. D., & Subramanyam, M. (2006). Indigenous health and socioeconomic status in India. PLoS Medicine, 3(10), e421. Sudarshan, H., & Seshadri, T. (2022). Health of Tribal People in Central India Tribal Development Report (pp. 85-157): Routledge India. Sundaram, K., Mohan, D., Advani, G., Sharma, H., & Bajaj, J. (1984). Alcohol abuse in a rural community in India. Part I: Epidemiological study. Drug and Alcohol Dependence, 14(1), 27-36. Vahedi, S. (2010). World Health Organization Quality-of-Life Scale (WHOQOLBREF): analyses of their item response theory properties based on the graded responses model. Iranian journal of psychiatry, 5(4), 140. Vaishnavi, R., Karthik, M. S., Balakrishnan, R., & Sathianathan, R. (2017a). Caregiver burden in alcohol dependence syndrome. Journal of addiction, 2017. Vaishnavi, R., Karthik, M. S., Balakrishnan, R., & Sathianathan, R. (2017b). Caregiver burden in alcohol dependence syndrome. Journal of addiction, 2017(1), 8934712. Vidyarthi, L. (1972). Problems and prospects of tribal development in India. Indian Anthropologist, 2(2), 80-93.
Conflict of interest: None
Role of funding source: None


